Statins & Azoles Interaction Checker
Select your statin and azole antifungal to see the interaction risk level.
Select your medications to see results
Combining azole antifungals with statins isn’t just a minor caution on a prescription label-it’s a potentially dangerous mix that can land you in the hospital. If you’re taking a statin for cholesterol and suddenly need an antifungal for a stubborn yeast infection or fungal pneumonia, you’re at risk for severe muscle damage, liver stress, and even life-threatening rhabdomyolysis. This isn’t theoretical. Thousands of patients experience this every year, and most don’t see it coming.
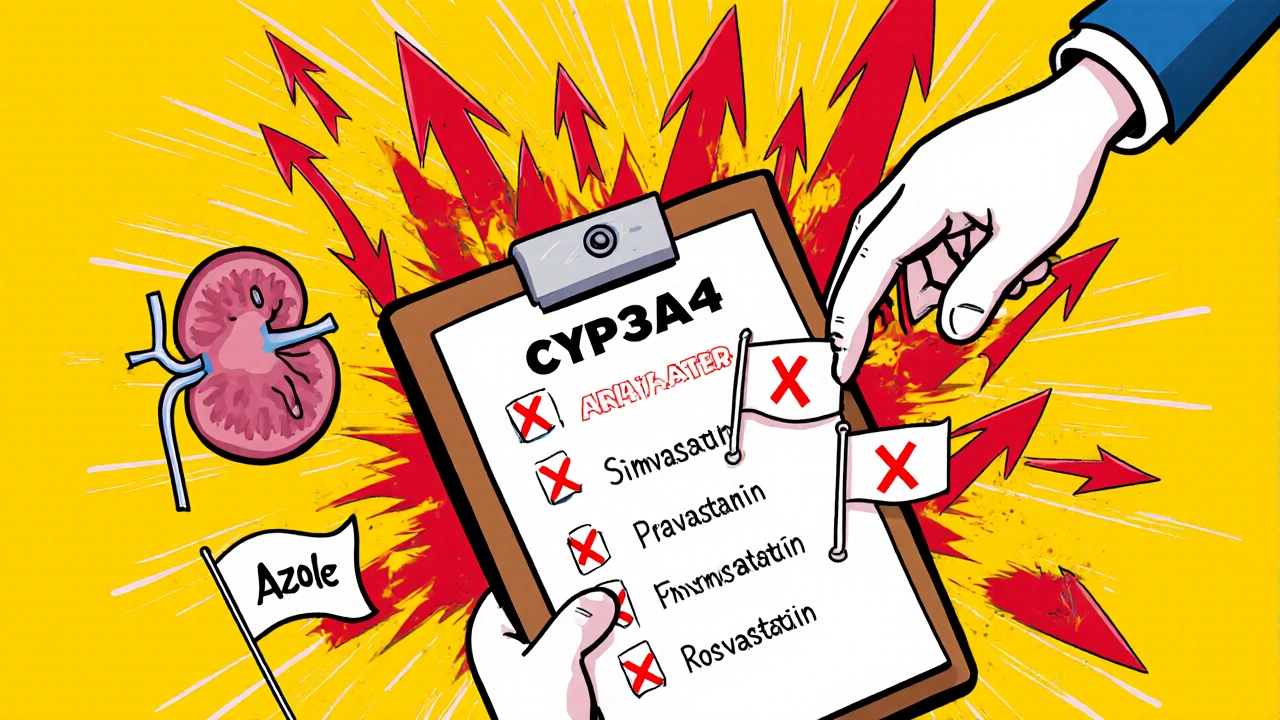
Why This Interaction Is So Dangerous
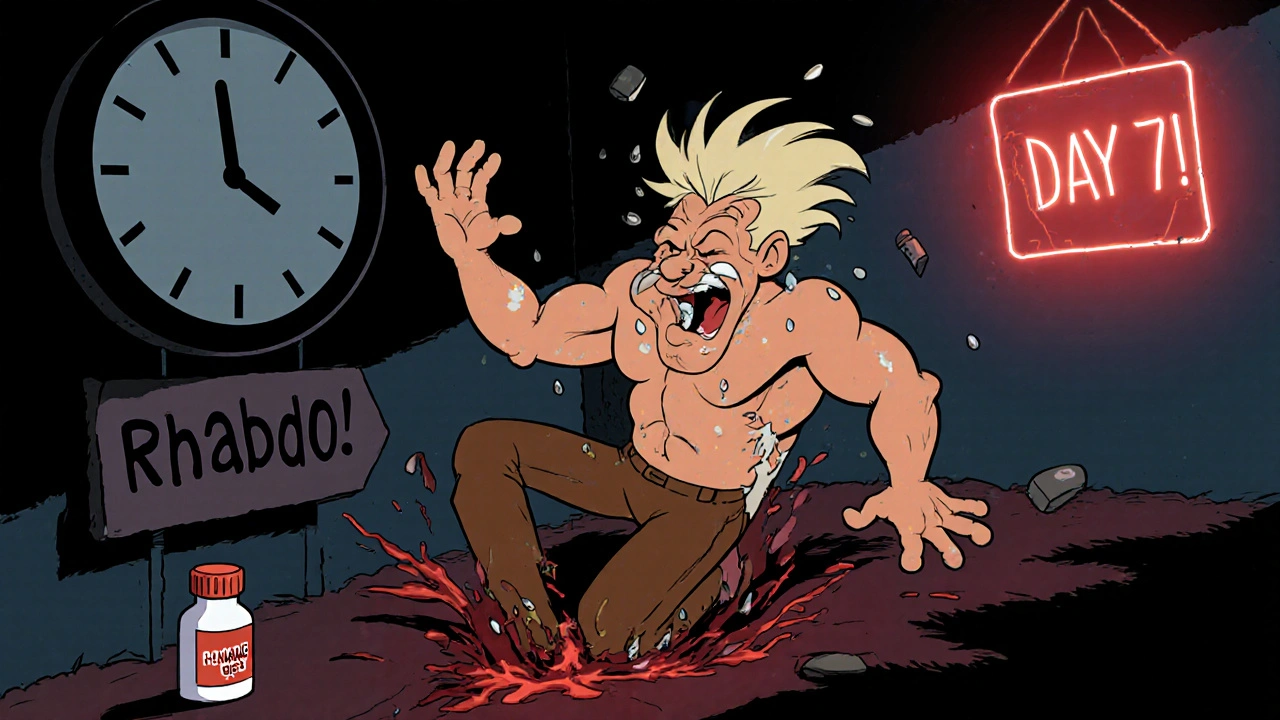
Both azole antifungals and certain statins are broken down by the same liver enzyme: CYP3A4. When you take an azole like itraconazole, ketoconazole, or posaconazole, it shuts down this enzyme like flipping a switch. That means your statin doesn’t get cleared from your body the way it should. Instead, it builds up-sometimes to 10 times normal levels.That spike in statin concentration is what turns mild muscle aches into full-blown muscle breakdown. The statin doesn’t just lower cholesterol-it also interferes with essential proteins your muscles need to function. When levels get too high, muscle cells start dying. Creatine kinase (CK) levels skyrocket, and your kidneys struggle to filter the debris. That’s rhabdomyolysis. It’s rare on statins alone, but with azoles? The risk jumps from less than 0.1% to over 5% in some cases.
Not All Statins Are Created Equal
If you’re on a statin and need an antifungal, your next move depends on which statin you’re taking. Some are far more dangerous when mixed with azoles than others.- Simvastatin and lovastatin are the worst offenders. Itraconazole can make simvastatin levels spike by over 10 times. That’s why the FDA says you can’t take more than 20 mg of simvastatin with any strong CYP3A4 inhibitor-and even that’s risky.
- Atorvastatin is moderately risky. Itraconazole can raise its levels by 3 times. Dose limits apply-stick to 20 mg or less if you must combine them.
- Pravastatin and rosuvastatin are your safest bets. They don’t rely on CYP3A4. Pravastatin is cleared mostly by the kidneys, and rosuvastatin uses a different liver pathway. With these, azole interactions are minimal-often under a 20% increase in blood levels.
- Fluvastatin is metabolized by CYP2C9, so it’s less affected by itraconazole but still at risk with fluconazole, which blocks that enzyme.
That’s why guidelines from the European Atherosclerosis Society and the American College of Cardiology now say: avoid simvastatin and lovastatin entirely if you’re on an azole antifungal. Switch to pravastatin or rosuvastatin instead.
What the Data Shows in Real Patients
Behind every warning label is a real person who got hurt.In the FDA’s adverse event database from 2015 to 2022, over 1,800 reports linked azole-azole combinations to muscle damage. Nearly half involved simvastatin and itraconazole. One Reddit thread from May 2023 had 30 pharmacists sharing stories: 67% had seen at least one patient develop muscle pain within two weeks of starting fluconazole while on simvastatin. One patient, a 73-year-old man on 40 mg simvastatin, developed muscle cramps so bad he couldn’t stand. His CK level hit 18,400 U/L-over 90 times the normal limit. He was hospitalized for five days.
A Mayo Clinic survey of 1,247 statin users found that when azoles were added, over 23% stopped their statin because of muscle pain. On statins alone? Only 8% quit. That’s a threefold increase in treatment failure-just from one added drug.
Who’s Most at Risk?
This isn’t a risk that affects everyone equally. Certain people are far more vulnerable.- People over 65: Aging liver and kidney function slow drug clearance. The American Geriatrics Society says to avoid all azole-statin combos in seniors.
- People with kidney disease: Pravastatin and rosuvastatin are safer, but even they can build up if kidneys aren’t working well.
- Those with SLCO1B1 gene variants: This genetic quirk reduces how well your liver takes up statins. Carriers have nearly five times higher risk of muscle damage when statins and azoles are combined.
- Those on high statin doses: The higher the statin dose, the more dangerous the interaction. A 40 mg dose of simvastatin is far riskier than 10 mg.
Doctors often miss these red flags. A 2022 survey found that while 72% of primary care doctors knew about this interaction, only 42% of nurse practitioners did. That gap means patients are getting prescriptions without proper screening.
What to Do If You’re on Both
If you’re already taking a statin and your doctor prescribes an azole antifungal, don’t panic-but don’t ignore it either.- Ask which statin you’re on. If it’s simvastatin or lovastatin, ask if you can switch to pravastatin or rosuvastatin during the antifungal course.
- Ask about alternatives. Is there a non-azole antifungal? Terbinafine (for nail fungus) or echinocandins (for systemic infections) don’t interfere with statins.
- Get a CK blood test before starting the antifungal and again after 7-10 days. If your CK rises more than 4 times the upper limit, stop the statin immediately.
- Watch for symptoms. Muscle pain, weakness, dark urine, or unexplained fatigue aren’t normal. Call your doctor right away.
- Don’t rely on timing. Taking your statin in the morning and azole at night won’t prevent this. The enzyme inhibition lasts days.
Liver Risks Are Often Overlooked
Muscle damage gets all the attention, but your liver is also at risk. Both statins and azoles can cause elevated liver enzymes. When combined, the risk of liver injury increases-especially with ketoconazole and itraconazole, which are known to be more hepatotoxic.The FDA requires liver function tests before starting statins and periodically after. When azoles are added, those tests become even more critical. A 2021 study in Pharmacoepidemiology and Drug Safety found that 12% of patients on combined therapy had ALT levels over three times normal, compared to 4% on statins alone.
If you’re on this combo, ask for liver enzyme checks at week 2 and week 4. If your enzymes climb, your doctor may need to stop one or both drugs.
What’s Changing in 2025?
The field is evolving. The 2023 European guidelines now recommend checking statin blood levels in high-risk patients on azoles-a practice that was rare just a few years ago. The FDA is also pushing for genetic testing for SLCO1B1 in patients who need long-term statin-azole combinations.Newer drugs like bempedoic acid (ETC-1002) are gaining ground. Approved in 2020, it lowers cholesterol without using CYP3A4. It’s not a statin, but it works similarly-and it doesn’t interact with azoles. By 2023, it made up 5.3% of new cholesterol prescriptions. That number is climbing.
Pharmacies are also getting better. Over 94% now have automated alerts that pop up when a prescriber tries to order simvastatin with itraconazole. But alerts aren’t foolproof. If the doctor overrides them, the risk remains.
Bottom Line: Know Your Meds
This isn’t about avoiding treatment. Fungal infections can be deadly. High cholesterol can lead to heart attacks. The goal isn’t to stop either-it’s to choose the safest path.If you’re on a statin and need an antifungal:
- Don’t assume your doctor knows the interaction.
- Ask: "Is my statin safe with this antifungal?" If they’re unsure, ask for a pharmacist consult.
- Switch to pravastatin or rosuvastatin if possible.
- Get blood tests before and during treatment.
- Report muscle pain or dark urine immediately.
Medication safety isn’t just about what’s prescribed-it’s about what you ask. You’re not being difficult. You’re protecting your body.
Can I take fluconazole with my statin?
Fluconazole is less risky than itraconazole or ketoconazole because it mainly inhibits CYP2C9, not CYP3A4. If you’re on pravastatin or rosuvastatin, fluconazole is generally safe. If you’re on simvastatin, lovastatin, or atorvastatin, the risk is moderate but still present. Your doctor may lower your statin dose or switch you temporarily. Always check with your provider before combining them.
What are the signs of statin-induced myopathy?
Early signs include unexplained muscle pain, tenderness, or weakness-especially in the shoulders, thighs, or lower back. You might feel unusually tired or have trouble climbing stairs. Dark or cola-colored urine is a red flag for muscle breakdown. If you notice any of these while taking an azole antifungal, stop the statin and call your doctor immediately.
Is there a statin that doesn’t interact with azoles at all?
Pravastatin and rosuvastatin have the lowest interaction risk. They don’t rely on CYP3A4 for metabolism. Pravastatin is cleared by the kidneys, and rosuvastatin uses a different liver transport system. Neither shows clinically significant increases in blood levels when taken with azoles. They’re the preferred choices when antifungal therapy is needed.
Can I take a natural antifungal instead?
Some people turn to garlic, coconut oil, or oregano oil for fungal infections. But these aren’t proven alternatives for systemic or serious infections. For nail fungus, terbinafine (a non-azole antifungal) is highly effective and doesn’t interact with statins. For oral thrush or invasive fungal infections, prescription antifungals are necessary. Don’t replace medical treatment with unproven remedies-especially when statins are involved.
How long does the interaction last after stopping the azole?
Azole antifungals can inhibit CYP3A4 for days to weeks after stopping, depending on the drug. Itraconazole’s effects can last up to two weeks. That means you should wait at least 7-14 days after finishing the antifungal before restarting a high-risk statin like simvastatin. Always check with your doctor before restarting.




Emily Gibson
October 29, 2025 AT 21:14Just had my doc switch me from simvastatin to rosuvastatin after I got prescribed fluconazole for a yeast infection. I didn’t even know this was a thing until I read this post. Seriously, if you’re on statins, ask your pharmacist before taking any antifungal. It’s not paranoia-it’s survival.
Also, dark urine? That’s not just dehydration. Call your doctor. Now.
Mirian Ramirez
October 30, 2025 AT 09:59Okay so I’m a nurse and I’ve seen this happen way too many times-elderly patients on simvastatin get fluconazole for thrush, then come in two weeks later with muscles so weak they can’t get out of a chair, and their CK is through the roof. And the worst part? They didn’t even know they were on a statin that could kill them. I’ve had to explain to families that their grandma’s hospitalization wasn’t ‘just old age’-it was a drug interaction that could’ve been avoided with one simple question. Please, please, please ask your provider what your meds do together. It’s not being difficult-it’s being smart. And if your doctor doesn’t know, ask for a pharmacist. They’re the real MVPs here.
Also, pravastatin and rosuvastatin are your friends. Don’t be afraid to ask for them. They’re not expensive, they’re not magic, they’re just… safer. And that’s enough.
Kika Armata
October 31, 2025 AT 21:29How is it even possible that this interaction isn’t universally mandated in EHR systems? The pharmacokinetics are textbook. CYP3A4 inhibition is not a novel concept-it’s been documented since the 1990s. The fact that we’re still seeing 1,800+ adverse event reports in the FDA database is a systemic failure of medical education, not a pharmacological surprise. If your prescriber doesn’t immediately recognize that itraconazole + simvastatin is a Class 1 contraindication, they shouldn’t be prescribing anything beyond aspirin. And yes, I’ve reviewed the literature. I’ve read the ACC guidelines. I’ve cross-referenced the FDA’s black box warnings. This isn’t opinion. It’s fact. And if you’re still taking simvastatin while on azoles, you’re not just at risk-you’re statistically negligent.
Also, natural remedies? Please. Garlic doesn’t cure aspergillosis. Stop embarrassing yourself.
Herbert Lui
November 2, 2025 AT 06:17There’s something haunting about how medicine works sometimes. We have all this data-genetic markers, enzyme pathways, real-world hospital stats-and yet, the person who’s most vulnerable is the one who doesn’t know the words to ask.
I think about that 73-year-old man with the CK of 18,400. He didn’t wake up one day thinking, ‘I wonder if my cholesterol pill will dissolve my muscles.’ He just took his meds like he was told. And now he’s got a scar on his body and a story he never wanted to tell.
Maybe the real problem isn’t the drugs. It’s the silence between the prescription and the panic.
We’re taught to trust. But maybe we should be taught to question-with kindness, with curiosity, with courage.
And if you’re reading this and you’re on a statin? Don’t wait for a crisis. Ask. Now.
Nick Zararis
November 3, 2025 AT 08:31PLEASE-ask your doctor: 'What statin am I on?'-then ask: 'Is it safe with azoles?'-then ask: 'Can we switch to pravastatin or rosuvastatin?'-then ask: 'Can I get a CK test before and after?'-then ask: 'What are the signs of muscle breakdown?'-then ask: 'What are the alternatives?'-then ask: 'Can I talk to the pharmacist?'-then ask: 'Is there a non-azole option?'-then ask: 'Will you write this down?'-then ask: 'Can I get a copy of this conversation?'-then ask: 'Will you email this to me?'-then ask: 'Can I print this?'-then ask: 'Can I show this to my family?'-then ask: 'Thank you.'-and then-DO IT.
Because if you don’t, someone else will have to write your obituary saying 'died of a drug interaction that was preventable.' And you don’t want that to be you.
Sara Mörtsell
November 5, 2025 AT 03:48People act like this is some secret medical conspiracy but it’s not-it’s just that doctors are overworked and patients are too scared to speak up. I got prescribed itraconazole last year while on 40mg simvastatin and my doctor didn’t say a word. I found this post on Reddit and panicked. Got my CK checked-was 2,800. They stopped the statin immediately. I’m alive because I googled. Not because my doctor cared. This isn’t healthcare-it’s a lottery. And the odds are stacked against people who don’t read.
Also, if you’re not testing your liver enzymes, you’re not treating-you’re gambling.
Rhonda Gentz
November 5, 2025 AT 21:54I’ve been on rosuvastatin for five years. Last month, I got a fungal sinus infection and was prescribed posaconazole. I didn’t panic. I didn’t Google. I just called my pharmacist. She said, ‘You’re good. Rosuvastatin doesn’t care about azoles.’ She was right. No issues.
That’s the power of knowing your meds. Not because you’re paranoid. But because you’re informed.
It’s not about fear. It’s about clarity.
And clarity is a gift you give yourself.
Alexa Ara
November 6, 2025 AT 06:09Hey everyone-just wanted to say this post gave me hope. I used to feel so alone in asking questions about my meds. Like I was being annoying. But reading this? I realized I’m not overreacting. I’m protecting myself.
I switched from simvastatin to pravastatin after my doc prescribed fluconazole. I felt so proud of myself for asking. And now I’m not scared anymore.
You’re not being difficult. You’re being brave.
And if you’re reading this and you’re scared to ask your doctor? Do it anyway. You’ve got this. I believe in you.
Love you all.
-Alexa
Olan Kinsella
November 7, 2025 AT 15:12Let’s be real. This isn’t about drugs. It’s about control. The system doesn’t want you to know that your life is hanging on a metabolic pathway. They want you to take the pill. Take the test. Take the label. Take the silence.
But here’s the truth: your body is not a machine. It’s a symphony. And when you force two toxic instruments to play together? The music dies.
I’ve seen people die from this. Not because they were careless. But because they trusted. And trust is the most dangerous drug of all.
Wake up.
They’re not saving you.
They’re selling you.
And you’re paying with your muscles.
And your liver.
And your life.
Kat Sal
November 8, 2025 AT 20:02My mom got hit with this exact combo last year-simvastatin + ketoconazole for a bad fungal infection. She was fine until she couldn’t lift her arms. We rushed her to the ER. Turned out her CK was 14,000. She spent a week in the hospital. Now she’s on rosuvastatin and it’s been smooth sailing.
But here’s the thing: if I hadn’t been the one to read this post and demand the CK test, she might not be here.
So if you’re reading this and you’re scared to ask your doctor-do it. Even if you’re nervous. Even if you think you’re bothering them. You’re not. You’re saving your life.
And if you’re a doctor reading this? Thank you. Please, please, please say something. Don’t assume they know.
Rebecca Breslin
November 8, 2025 AT 21:01Everyone’s acting like this is new news. It’s not. I’ve been warning people on my pharmacy forum for years. Itraconazole + simvastatin = bad. End of story. If you’re on simvastatin and your doctor gives you an azole, you have three choices: switch statins, switch antifungal, or don’t take either. No in-between. No ‘maybe.’ No ‘I’ll be careful.’
And yes, I’ve seen the Mayo Clinic data. I’ve read the FDA alerts. I’ve reviewed the case reports. This isn’t theory. It’s a pattern. And if you’re still on simvastatin? You’re playing Russian roulette with your muscles.
Pravastatin or rosuvastatin. Period.
Kierstead January
November 9, 2025 AT 15:40Oh wow. Another ‘medical advice’ post from someone who read a PubMed abstract and thinks they’re a doctor now. Let me guess-you also think vaccines cause autism and 5G is mind control? Classic. This isn’t ‘dangerous,’ it’s just another fear-mongering article designed to make people distrust their doctors. The real risk? Not taking your statin. That’s what kills people. Not azoles. Not CYP3A4. Not CK levels. Your fear.
Stop Googling. Take your pill. Be grateful you’re alive.
And if you’re on pravastatin? Good for you. You’re one of the 5% who actually listen to their doctor. The rest of you? You’re just adding to the noise.
Imogen Levermore
November 10, 2025 AT 07:56Wait… so you’re telling me the FDA and Big Pharma are hiding this? Because if this interaction is so dangerous, why aren’t there giant warning signs on every bottle? Why aren’t we all being scanned for SLCO1B1 at birth? Why is this only being talked about now? Because it’s not about safety. It’s about profit. Simvastatin is cheaper. Rosuvastatin? Patent expired in 2026. They’re milking the old stuff while you sleep.
And don’t even get me started on ‘pharmacists.’ They’re just corporate agents with white coats.
Trust no one. Not your doctor. Not your pharmacist. Not this post.
Just take garlic. And pray.
💜
Chris Dockter
November 11, 2025 AT 02:23This is why you don’t trust doctors. They don’t know shit. My cousin died from this. Simvastatin. Fluconazole. No one warned him. He was 52. Just went to bed. Never woke up. Autopsy said rhabdo. Liver failure. No one said a word. Now I only take herbal stuff. Turmeric. Black seed oil. No pills. No science. Just vibes.
They lied to us. All of them.
Gordon Oluoch
November 12, 2025 AT 23:08Another emotional appeal from someone who doesn’t understand pharmacology. The risk of rhabdomyolysis from statin-azole interaction is statistically insignificant compared to the cardiovascular benefit of statins. You’re trading a 0.1% risk for a 20% reduction in heart attack. That’s not a trade-it’s a win. The fact that you’re terrified of a 5% increase in a rare event suggests you have no grasp of relative risk. Your fear is not a valid clinical argument. Your anxiety is not a medical guideline. Stop letting anecdotes override data.
And yes, the liver enzyme elevations are real-but they’re transient. Most resolve on their own. You’re not dying from a 12% ALT rise. You’re dying from not taking your statin.
Stop scaring people. Start educating them. Or at least, stop being so dramatic.
Emily Gibson
November 13, 2025 AT 16:16Rebecca, you’re right that the stats favor statins-but you’re ignoring the human cost. That 5% isn’t a number. It’s a 73-year-old man who can’t walk. A 65-year-old woman who can’t hug her grandkids. A single mom who can’t work for six months because her muscles turned to jelly.
And if your doctor doesn’t know the difference between simvastatin and rosuvastatin? That’s not your fault. That’s the system’s failure.
Don’t reduce a person’s suffering to a risk-benefit ratio. That’s not medicine. That’s math.