When you’re over 65 and taking blood pressure medication, standing up too fast can feel like a gamble. One moment you’re fine, the next you’re seeing stars, gripping the countertop, or worse-lying on the floor after a fall. This isn’t just bad luck. It’s orthostatic hypotension, a drop in blood pressure when you stand, and it’s more common-and more dangerous-than most people realize.
One in four older adults with high blood pressure experiences this. And here’s the twist: the very drugs meant to protect your heart might be making you more likely to fall. But the good news? You don’t have to accept it. With the right medication choices and simple daily habits, you can manage your blood pressure without putting yourself at risk.
What Is Orthostatic Hypotension-and Why Does It Matter?
Orthostatic hypotension happens when your blood pressure drops sharply within three minutes of standing. The official definition? A drop of 20 mm Hg in systolic pressure or 10 mm Hg in diastolic pressure. That’s not a minor dip. It means less blood reaches your brain, and that’s what causes dizziness, blurred vision, or fainting.
It’s not rare. Studies show 3% to 26% of older adults with hypertension have it. The risk climbs with age. Why? As you get older, your body’s natural pressure regulators slow down. Your heart doesn’t pump as fast when you stand. Your blood vessels don’t squeeze back quickly enough. Your kidneys don’t hold onto salt and fluid like they used to. These changes make it harder for your body to keep blood flowing upward when you move from lying down to standing.
But here’s what most doctors used to get wrong: they thought treating high blood pressure too aggressively would make orthostatic hypotension worse. That’s not true. The landmark SPRINT trial and multiple follow-up studies found that older adults who aimed for lower blood pressure targets-below 120 mm Hg-actually had less orthostatic hypotension than those with looser targets. Aggressive treatment didn’t increase falls. It lowered heart attacks, strokes, and death.
Which Blood Pressure Medications Are Riskiest?
Not all blood pressure pills carry the same risk. Some are much more likely to trigger orthostatic hypotension than others. If you’re over 65, knowing which ones to watch out for can save you from a fall.
Alpha blockers like doxazosin and terazosin are the worst offenders. Up to 28% of older adults taking them experience orthostatic hypotension. They relax blood vessels too much, too fast. That’s why the American Geriatrics Society Beers Criteria calls them “potentially inappropriate” for seniors.
Beta-blockers like metoprolol and atenolol are next on the list. They slow your heart rate, which makes it harder for your body to compensate when you stand. Studies show they more than double the risk of sustained low blood pressure upon standing.
Diuretics (water pills) like hydrochlorothiazide and furosemide can cause dehydration and low blood volume. That’s a double hit: less fluid in your system, plus blood vessels that don’t respond well to standing.
Central sympatholytics like clonidine and methyldopa also carry high risk. They work on your brain to reduce nerve signals that keep blood pressure up-so when you stand, your body doesn’t get the signal to tighten up.
Even some calcium channel blockers can be tricky. Diltiazem and verapamil, especially in older people with slower liver function, can cause bigger drops. But amlodipine and isradipine? Much safer. They work slowly, giving your body time to adjust.
Which Medications Are Safest for Older Adults?
The good news? Some blood pressure drugs actually protect against orthostatic hypotension.
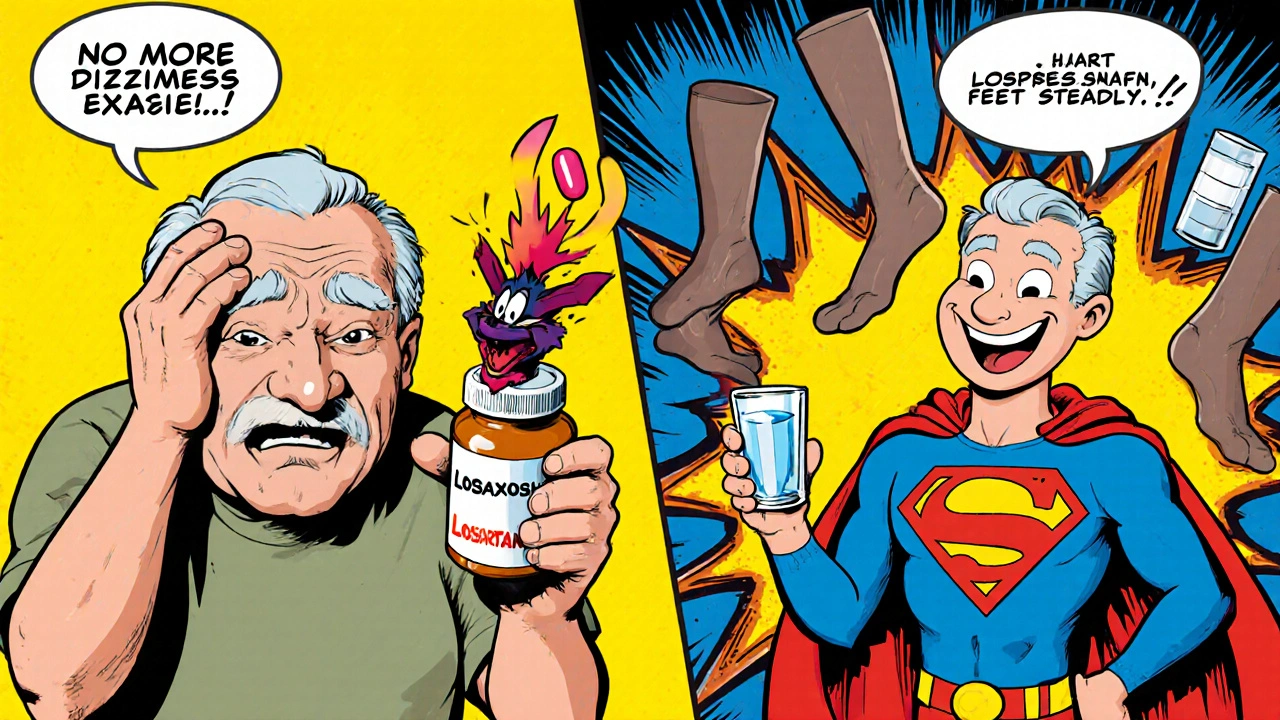
ACE inhibitors (like lisinopril) and ARBs (like losartan or valsartan) are the top choices. Multiple studies show they cause the least orthostatic hypotension-only 8% to 10% of users experience it. Some research even suggests they may help prevent it. That’s why, in 2023, 38% of new prescriptions for seniors over 65 were ACE inhibitors or ARBs-up from 32% just three years ago.
Why do they work better? They don’t cause sudden, wide vessel dilation. They don’t blunt your heart’s natural response. And they’re gentle on kidney function, which matters as you age.
Thiazide diuretics, if needed, can still be used-but only at low doses and with careful monitoring. Sometimes, switching from a high-risk drug to an ARB alone can cut dizziness and falls by 65%, according to clinical practice data.
What to Do Before You Stand Up
Medication changes help-but so do simple habits. You don’t need fancy equipment. Just awareness and timing.
- Stand up slowly. Don’t jump from lying down to standing. Sit on the edge of the bed for 30 seconds first.
- Wait 1-2 minutes after using the toilet or after eating a big meal. Blood rushes to your gut after eating, which can drop pressure further.
- Wear compression stockings. They help push blood back up from your legs.
- Stay hydrated. Drink water before getting up, especially in the morning or after sweating.
- Avoid alcohol. It widens blood vessels and makes drops worse.
- Exercise your legs before standing. Wiggle your toes, flex your calves. It helps pump blood upward.
Practice these moves several times a day. Most people notice less dizziness within 2 to 4 weeks. It’s not magic-it’s training your body to respond better.
When to Talk to Your Doctor
If you’ve had a fall, feel lightheaded daily, or get dizzy after standing up, don’t wait. Ask for a standing blood pressure check. Your doctor should measure your pressure while you’re lying down, then again after 1 and 3 minutes of standing. That’s the only way to know for sure if orthostatic hypotension is happening.
Don’t assume your meds are fine just because your blood pressure looks good at the clinic. That’s supine pressure. You need to know what happens when you move.
Ask: “Could any of my medications be causing dizziness when I stand?” Bring your full list-even supplements and over-the-counter drugs. Some painkillers, antidepressants, and even antihistamines can make it worse.
If you’re on an alpha blocker or a high-dose beta-blocker, ask if switching to an ARB or ACE inhibitor is possible. Many seniors feel better within weeks after the switch.

What About Medications Just for Orthostatic Hypotension?
Drugs like midodrine, droxidopa, or fludrocortisone exist to treat orthostatic hypotension directly. But they’re not first-line for older adults with high blood pressure. Why? They can raise your blood pressure too much when you’re lying down, increasing stroke risk. They’re usually reserved for people with severe symptoms who’ve already optimized their antihypertensives and lifestyle habits.
Most doctors avoid them unless absolutely necessary. The goal isn’t to treat the symptom with another drug-it’s to fix the root cause: the wrong blood pressure medication.
The Bigger Picture: Safer Blood Pressure Control Is Possible
The old thinking was: lower blood pressure = more falls. That’s been proven wrong. The real danger isn’t low blood pressure-it’s the wrong way to get there.
High blood pressure kills. But so do falls. You don’t have to choose one over the other. With the right drugs-like ARBs and ACE inhibitors-and smart daily habits, you can protect your heart and stay steady on your feet.
By 2025, personalized blood pressure management is becoming standard. Doctors are learning to look beyond the clinic number. They’re checking how you feel when you stand. They’re asking about dizziness. They’re reviewing every pill you take.
You’re not powerless. Ask the right questions. Know your meds. Move slowly. Your next step might be as simple as asking your doctor: “Could I switch to a safer blood pressure pill?”
Can blood pressure medication cause dizziness when standing?
Yes, certain blood pressure medications can cause dizziness when standing due to orthostatic hypotension. Alpha blockers, beta-blockers, diuretics, and central sympatholytics are the most likely culprits. These drugs can lower blood pressure too much when you change position, reducing blood flow to the brain. ACE inhibitors and ARBs carry much lower risk and are often preferred for older adults.
Is it safe to lower blood pressure aggressively in older adults?
Yes, and it’s often safer than leaving it high. Studies like the SPRINT trial show that older adults who aim for a systolic blood pressure below 120 mm Hg have fewer heart attacks, strokes, and deaths-and no increase in falls or orthostatic hypotension compared to those with higher targets. The key is choosing the right medications and adjusting slowly under medical supervision.
Which blood pressure meds are safest for seniors?
ACE inhibitors (like lisinopril) and ARBs (like losartan or valsartan) are the safest choices for older adults at risk of orthostatic hypotension. They have the lowest incidence of dizziness upon standing-around 8-10%-and may even help prevent it. Amlodipine and isradipine are also safer calcium channel blockers compared to diltiazem or verapamil.
How can I prevent dizziness when standing up?
Stand up slowly: sit on the edge of the bed for 30 seconds before standing. Drink water before getting up, especially in the morning. Wear compression stockings. Avoid large meals and alcohol before standing. Exercise your legs by wiggling your toes or flexing your calves before rising. Practice these steps daily-most people see improvement in 2 to 4 weeks.
Should I stop my blood pressure medicine if I feel dizzy?
No. Stopping your medication without medical advice can raise your blood pressure dangerously and increase your risk of stroke or heart attack. Instead, talk to your doctor. They can check if your dizziness is from orthostatic hypotension and may switch you to a safer medication or adjust your dose. Never stop or change your pills on your own.
Do I need special tests to check for orthostatic hypotension?
Yes. A simple standing blood pressure test is all you need. Your doctor should measure your blood pressure while you’re lying down, then again after you stand up at 1 and 3 minutes. A drop of 20 mm Hg systolic or 10 mm Hg diastolic confirms orthostatic hypotension. This test should be part of any routine checkup for seniors on blood pressure meds.
If you’re managing high blood pressure as an older adult, your goal isn’t just to hit a number. It’s to live safely, steadily, and without fear of falling. The right medication, paired with small daily changes, can make all the difference.





King Over
November 19, 2025 AT 11:11Been on amlodipine for 5 years. Never dizzy. Just stand slow. Done.
Michael Fessler
November 21, 2025 AT 10:40As a geriatric pharmacist, I see this daily. Alpha blockers like doxazosin are absolute landmines in seniors. The Beers Criteria isn't just a suggestion-it's a lifesaver. I always push for ARBs first. Lisinopril's fine too, but if they're diabetic or have microalbuminuria? Losartan's the gold standard. And don't forget: hydration + compression socks = 70% reduction in syncopal episodes. No magic, just physiology. Also, watch for OTC antihistamines-diphenhydramine is a silent fall enabler.
Johannah Lavin
November 23, 2025 AT 07:21OMG YES THIS. 😭 I watched my grandma fall 3 times last year because she was on terazosin. We switched her to valsartan and she’s now walking the dog every morning without clutching the railing. I cried when she said, ‘I don’t feel like I’m gonna pass out anymore.’ 🥹❤️ Also, compression socks are the unsung heroes of aging. Get the knee-high ones with 20-30 mmHg. They’re not sexy but they’re magic.
daniel lopez
November 24, 2025 AT 04:55SPRINT trial? That’s Big Pharma’s lie to sell more pills. They don’t want you to know that low BP = brain damage over time. Your arteries need pressure to stay elastic! They’re pushing ‘under 120’ like it’s a religion. My uncle’s BP is 135/80-he’s 82, runs marathons, eats butter. He’s fine. The real danger? Doctors overtreating. And don’t even get me started on ‘compression stockings’-that’s just a scam to sell useless socks. Real men don’t wear them.
Nosipho Mbambo
November 25, 2025 AT 15:51So… you’re saying I shouldn’t stand up fast? And that my 75-year-old dad’s dizziness isn’t just ‘getting old’? Wow. I didn’t know. Thanks? I guess? I mean… I read the article. But I’m tired. And I didn’t get coffee yet. So I’m not sure I’m processing this. 🤷♀️
Katie Magnus
November 25, 2025 AT 16:15Ugh. Another ‘safe med’ list. Like anyone cares. My aunt took lisinopril and got a cough so bad she had to quit. So now she’s on amlodipine and still dizzy. So what’s the point? It’s all a scam. The real fix? Stop taking pills. Just lie down. Forever. 🙄
Ravinder Singh
November 27, 2025 AT 11:12Bro, this is gold. 🙌 I'm from India, my dad's on metoprolol, and he's been stumbling around like a drunk penguin. I showed him this article-he cried. We switched him to telmisartan last week. No dizziness. He even danced at my sister's wedding. 🎉 Also, the toe-wiggling thing? We do it before he gets up. He says it feels like his legs remember how to work. Love this. Keep sharing.
Russ Bergeman
November 29, 2025 AT 03:17Wait, so you’re telling me that my mom’s 3 falls in 6 months were caused by hydrochlorothiazide? And not because she’s ‘just clumsy’? And that her doctor didn’t even check her standing BP? That’s malpractice. You’re lucky she didn’t die. She’s on lisinopril now. But I’m still mad. Why didn’t anyone tell us this before?
Dana Oralkhan
November 30, 2025 AT 14:27This is so important. I’m a nurse and I’ve seen too many seniors get labeled ‘fall risk’ and then get put on more meds that make it worse. The real solution? Slow down. Hydrate. Move your feet. And ask your doctor: ‘Which of these pills is making me dizzy?’ It’s not weak to ask. It’s smart. And if they get defensive? Find a new doctor. You deserve to feel safe in your own body.
Nicole Ziegler
December 1, 2025 AT 10:14compression socks 🤍
Bharat Alasandi
December 2, 2025 AT 11:08Man, this is the kind of post that saves lives. I shared it with my uncle in Delhi-he’s on doxazosin. He called me crying. Said he thought he was just ‘getting old.’ Now he’s switching to valsartan. I told him: ‘Your legs aren’t broken, they’re just forgotten.’ He’s gonna start wiggling his toes every morning. Small steps. Big wins. 🙏
Kristi Bennardo
December 3, 2025 AT 11:59While the information presented here is superficially compelling, it lacks critical nuance regarding the heterogeneity of elderly populations. The SPRINT trial excluded individuals with dementia, history of stroke, and frailty-yet these are precisely the cohorts most vulnerable to orthostatic hypotension. To generalize these findings as universally applicable is not merely irresponsible-it is ethically indefensible. Furthermore, the recommendation to discontinue beta-blockers ignores their proven cardioprotective effects in post-MI patients. This article reads like a marketing pamphlet for ARBs, not clinical guidance.
Shiv Karan Singh
December 5, 2025 AT 02:27Everyone’s obsessed with ARBs and ACEis. But have you checked the cost? In the U.S., losartan’s $4. Valsartan? $120. So who’s really benefiting? The pharmacy benefit managers. The real solution? Stop taking meds entirely. Eat garlic. Walk barefoot. Let your body find balance. You don’t need a pill to live. You need to stop trusting doctors.