For people managing diabetes, checking blood sugar used to mean pricking your finger several times a day-sometimes more. It was messy, painful, and only gave you a single snapshot in time. You’d see a number, guess what happened before it, and hope you weren’t heading for a crash or spike. But that’s not how it works anymore. Today, CGMs are changing everything. They don’t just tell you your glucose level-they show you the story behind it.
What CGMs Really Do (And Why They’re No Longer Optional)
Continuous Glucose Monitors, or CGMs, are small sensors worn on the skin that measure glucose in the fluid between your cells every five minutes, day and night. Unlike fingersticks, they don’t just give you one number. They show you trends: Is your sugar rising fast? Dropping overnight? Spiking after lunch? This is called time in range-the percentage of hours you spend between 70 and 180 mg/dL. Studies show that for every 10% increase in time in range, your risk of eye, kidney, and nerve damage drops by 64%. That’s not a small gain. It’s life-changing. The American Diabetes Association now says CGMs should be used by everyone with Type 1 diabetes, anyone with Type 2 on insulin, pregnant people with diabetes, older adults at risk for low blood sugar, and even children from the moment they’re diagnosed. This isn’t a luxury anymore. It’s the new standard of care. Three systems dominate the market: Dexcom G7, Abbott FreeStyle Libre 3, and Medtronic Guardian 4. Abbott’s Libre 3 has a MARD score of 8.1%, meaning it’s accurate within about 8% of lab results. Dexcom’s G7 is smaller, lasts 10 days, and connects directly to Apple Watches. Medtronic’s Guardian 4 works best when paired with their insulin pumps. Then there’s Glucotrack-an experimental implantable sensor that measures glucose directly from blood, not interstitial fluid. That means no lag time. No 15-minute delay between your real blood sugar and what the device shows. It’s still in trials, but early results show a MARD of 7.7%, even better than current external sensors.Smart Pens: The Quiet Partner in Your Diabetes Routine
While CGMs tell you what’s happening, smart insulin pens help you respond. The InPen by Medtronic is one of the most common. It’s a regular insulin pen, but it has Bluetooth and a built-in memory. Every time you inject, it records the dose, time, and even the type of insulin. It can sync with your CGM and suggest a dose based on your current glucose level, carb intake, and recent trends. It doesn’t auto-deliver insulin like a pump-but it cuts down guesswork. Yet adoption is low. Only 15% of insulin users use smart pens, according to 2025 data from ADCES. Why? Cost. Complexity. Lack of awareness. Many doctors still hand out pens without explaining how to use them digitally. But for people who hate pumps or want more control without surgery, smart pens are a powerful middle ground. They turn a simple tool into a data source-linking insulin use directly to glucose patterns.Apps: The Brain Behind the Data
All this data means nothing if you can’t make sense of it. That’s where apps come in. mySugr, One Drop, and Glucose Buddy let you log meals, exercise, stress, and insulin doses alongside your CGM readings. Some even let you share trends with your care team remotely. But here’s the catch: not all apps work with all devices. Only 43% of third-party diabetes apps can connect to all major CGMs. If you’re using a Dexcom G7, your app might not talk to your Abbott Libre 3. That’s frustrating. It’s like having a fitness tracker that won’t sync with your phone. Before you buy an app, check its compatibility list. Look for ones that integrate with your specific CGM model. The best apps don’t just display graphs-they explain them. They flag patterns: “Your sugar spikes after pasta on weekends.” Or, “You’re going low at 3 a.m. three nights a week.” That kind of insight turns data into action. One user on Reddit said their app showed them their morning highs weren’t from eating too much-they were from overnight lows followed by a rebound. Once they adjusted their bedtime snack, their A1c dropped from 9.2% to 6.8% in four months.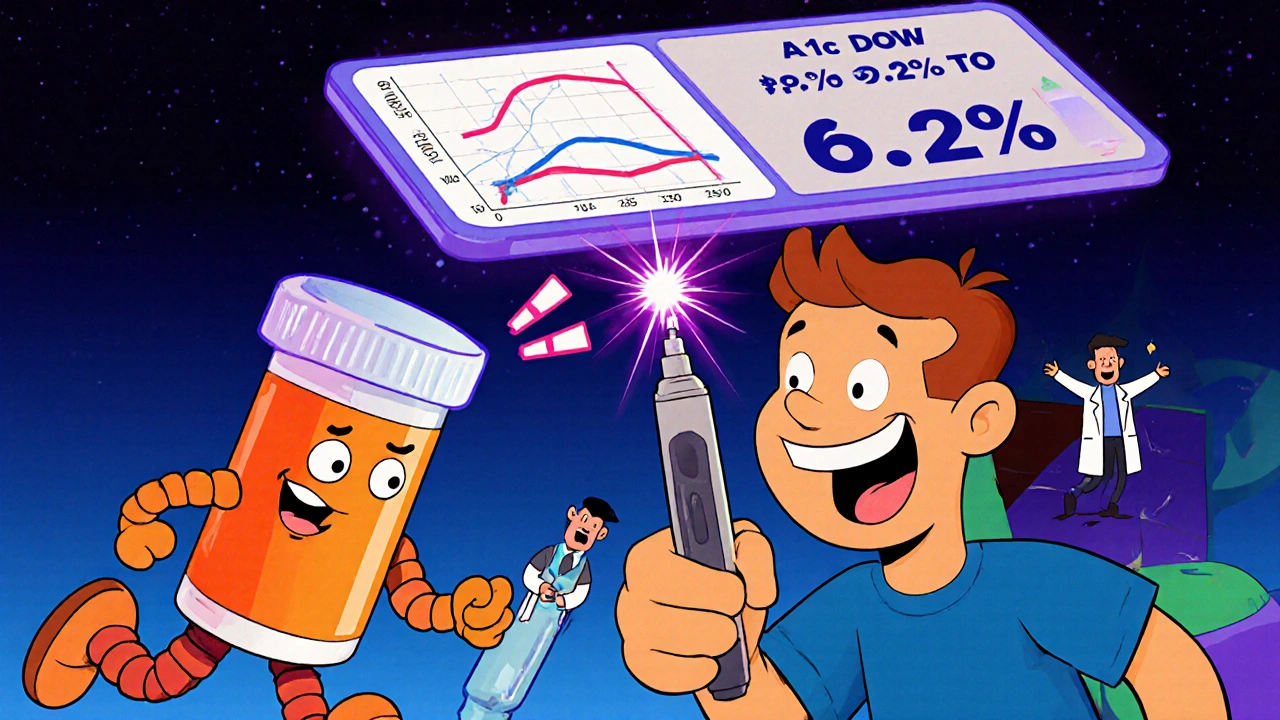
Real-Life Wins (And the Real Problems)
People aren’t just using this tech-they’re thriving. A 2025 remote CGM program in underserved areas helped participants lower their A1c from 10.4% to 7.5% in just three months. Foot wounds healed 72% faster than in non-CGM users. Sleep improved because alarms woke people before their sugar crashed. Anxiety dropped. One survey found 78% of users slept better knowing they’d get an alert if their glucose went too low. But it’s not perfect. Sensor adhesion is a big issue-45% of users say their sensors fall off during sweat, showers, or workouts. Insurance is another hurdle. Even with coverage, 37% of commercially insured patients get denied prior authorizations. For those without insurance, out-of-pocket costs can hit $300 a month. That’s not affordable for many. And then there’s data overload. New users often get bombarded with alerts. One study found 68% of people turned off all alarms at first because they were overwhelmed. The fix? Personalize. Set your high and low thresholds based on your life-not a default setting. Night-shift workers need different alerts than office workers. Athletes need different ones than sedentary people. The ADA now recommends customizing alerts, not just accepting the factory settings.What’s Coming Next
The future is faster, smarter, and more connected. Machine learning models are now predicting glucose spikes up to 30 minutes ahead with 89% accuracy. Dexcom and EarlySense are launching this feature in early 2026. It won’t just warn you-it’ll tell you why: “Your sugar will rise in 20 minutes because of your morning coffee and lack of sleep.” Vaxess Technologies is testing a needle-free patch for semaglutide (Ozempic), which could make weekly injections a thing of the past. And Glucotrack’s implantable sensor-about the size of three nickels-is targeting a U.S. launch in 2028. If it works, it could prevent 12,000-15,000 severe low-blood-sugar events every year in the U.S. alone. But the biggest challenge isn’t tech. It’s access. A 2025 JAMA study found 63% of CGM systems had data security flaws. And 41% of low-income patients still can’t get them, even after Medicare expanded coverage. Technology won’t help if it’s only available to those who can afford it.
How to Get Started
If you’re thinking about switching to a CGM, here’s what to do:- Ask your doctor if you qualify. Medicare and many insurers now cover CGMs for Type 2 diabetes on insulin.
- Check what devices your insurance covers. Dexcom, Abbott, and Medtronic have different contracts.
- Don’t skip training. 78% of people who stick with CGMs complete formal education. Those who don’t often quit within 30 days.
- Customize your alerts. Start with conservative settings, then adjust based on your life.
- Pair it with an app that works with your device. Look for one that shows trends, not just numbers.
Is This Right for You?
You don’t need to be on insulin to benefit. If you’re struggling with unpredictable highs and lows, if you’re tired of fingersticks, if you want to sleep through the night without fear-CGMs can help. Smart pens add clarity to your insulin use. Apps turn noise into understanding. This isn’t about being high-tech. It’s about being in control. About knowing your body better than ever before. About turning guesswork into confidence. The tools are here. The science is solid. The question isn’t whether you should use them-it’s when you’ll start.Can I use a CGM if I have Type 2 diabetes and don’t take insulin?
Yes, but coverage depends on your insurance and doctor’s recommendation. The American Diabetes Association’s 2025 guidelines now recommend CGMs for people with Type 2 diabetes who are at risk for hypoglycemia-even if they’re not on insulin. For example, if you’re taking sulfonylureas or glinides, which can cause low blood sugar, a CGM can help prevent dangerous drops. Some insurers require a trial of fingerstick monitoring first, but more are approving CGMs without insulin use, especially if you have frequent highs or lows.
How often do I need to replace my CGM sensor?
It depends on the device. Dexcom G7 lasts 10 days, Abbott FreeStyle Libre 3 lasts 14 days, and Medtronic Guardian 4 sensors last 7 days. Some newer models, like the Eversense E3, are implanted and last up to 6 months. The Abbott Libre 3 is the most popular because it’s small, disposable, and doesn’t require a separate transmitter. Most sensors are designed to be worn during showers and exercise, but adhesion can be an issue in hot weather or with heavy sweating. Always follow the manufacturer’s instructions for placement and care.
Are CGMs accurate during rapid blood sugar changes?
Traditional CGMs measure glucose in interstitial fluid, not blood, so there’s a lag of 5 to 15 minutes. That means during fast drops or spikes-like after eating or exercising-the reading might not match your real-time blood sugar. For most daily decisions, this lag is fine. But if you’re treating a low or about to exercise, always confirm with a fingerstick if you feel symptoms that don’t match your CGM. Implantable sensors like Glucotrack, still in development, aim to eliminate this lag by measuring directly from blood.
Can I use a CGM and smart pen together?
Yes, and many people do. The InPen smart pen syncs with Dexcom and Abbott CGMs to give you insulin dose suggestions based on your current glucose level, carb intake, and recent trends. It doesn’t replace a pump, but it makes insulin dosing more precise. You still inject manually, but you’re doing it with data, not guesswork. This combo is especially helpful for people who want the control of insulin without the complexity of a pump.
Do I need to pay for a diabetes app?
Most major apps like mySugr and One Drop are free to download and use basic features. Premium versions cost around $5-$10 per month and unlock advanced analytics, coaching, and sharing with your care team. But the key is compatibility-not cost. Make sure the app works with your specific CGM model. Some apps only connect to Dexcom, others only to Libre. Check the app’s website before downloading. You can often use the manufacturer’s own app for free (like Dexcom Clarity or LibreLink), which is usually the most reliable option.
What if my insurance denies my CGM?
Denials are common, especially for Type 2 diabetes patients not on insulin. First, ask your doctor to write a detailed letter of medical necessity, citing ADA 2025 guidelines. Include your history of hypoglycemia, A1c levels, or frequent highs. If denied, appeal. Many patients succeed on the second try. Some manufacturers offer patient assistance programs. Abbott’s Libre program, for example, provides free sensors for uninsured or underinsured patients who qualify. Don’t give up-advocacy works.
Can CGMs help with weight loss?
Yes, indirectly. By showing you how food affects your glucose, CGMs help you identify which meals spike your sugar and lead to fat storage. A 2025 study at the ADA conference showed that combining CGM data with semaglutide (Ozempic) helped Type 1 diabetes patients lose an average of 18 pounds over six months-without increasing low-blood-sugar events. People who used CGMs to adjust their eating patterns lost more weight than those who didn’t, even without dieting. It’s not a weight-loss tool, but it’s a powerful guide for making smarter food choices.



Jessica Chambers
November 14, 2025 AT 14:29Shyamal Spadoni
November 15, 2025 AT 05:57Ogonna Igbo
November 15, 2025 AT 20:24BABA SABKA
November 16, 2025 AT 07:14Chris Bryan
November 16, 2025 AT 23:09Jonathan Dobey
November 17, 2025 AT 01:01ASHISH TURAN
November 18, 2025 AT 15:09Ryan Airey
November 20, 2025 AT 02:01Hollis Hollywood
November 21, 2025 AT 18:55Aidan McCord-Amasis
November 22, 2025 AT 07:00Adam Dille
November 22, 2025 AT 17:08Katie Baker
November 23, 2025 AT 13:29John Foster
November 24, 2025 AT 11:50Edward Ward
November 26, 2025 AT 11:03Andrew Eppich
November 26, 2025 AT 12:39Jessica Chambers
November 28, 2025 AT 11:31