When your baby’s skin is dry, red, and itchy, it’s easy to think it’s just a rash. But what if that rash is the first sign of something bigger? For many children, eczema isn’t just a skin problem-it’s the starting point of a chain reaction that can lead to food allergies, asthma, and hay fever. This progression is called the atopic march, and understanding it changes how you care for your child’s skin from day one.
What Is the Atopic March, Really?
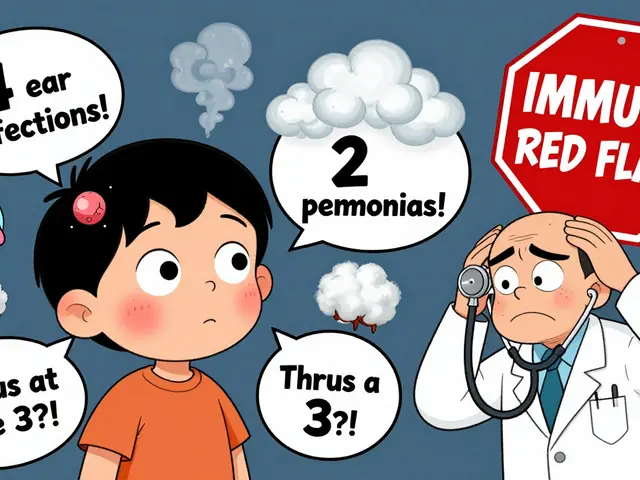
The atopic march used to be taught like a straight line: eczema first, then food allergies, then asthma, then allergic rhinitis. But that’s not how it works for most kids. Recent studies show only about 3.1% of children with eczema follow that exact path. The real story is messier-and more important. Most kids with eczema don’t go on to develop asthma. In fact, only about 25% do. But here’s the key: if your child has severe eczema, their risk jumps. One study found that children with severe eczema were more than 60% more likely to develop asthma than those with mild cases. And if they do get asthma, there’s a 74-81% chance they’ll also develop allergic rhinitis by age three. The real shift in science is this: it’s not about inevitable progression. It’s about risk. Some kids are genetically wired to develop multiple allergic conditions. Others aren’t. The goal isn’t to fear eczema-it’s to know which kids need extra attention.Why Skin Barrier Breakdown Is the Starting Point
Your skin isn’t just a cover. It’s a shield. And in babies with eczema, that shield has cracks. These aren’t just dry patches-they’re openings where allergens like peanut proteins, egg, and cow’s milk can slip in through the skin. This is where the dual-allergen exposure hypothesis comes in. When allergens enter through broken skin, the immune system learns to see them as threats. That’s sensitization. But when those same allergens are eaten early and often, the immune system learns they’re safe. That’s tolerance. The LEAP study proved this. Babies with severe eczema who were given peanut protein regularly before age one had an 86% lower chance of developing a peanut allergy by age five. But if they never ate peanut and had cracked skin? Their risk skyrocketed. It’s not about avoiding allergens. It’s about controlling how your child is exposed.The Genetic Clues: Filaggrin and Beyond
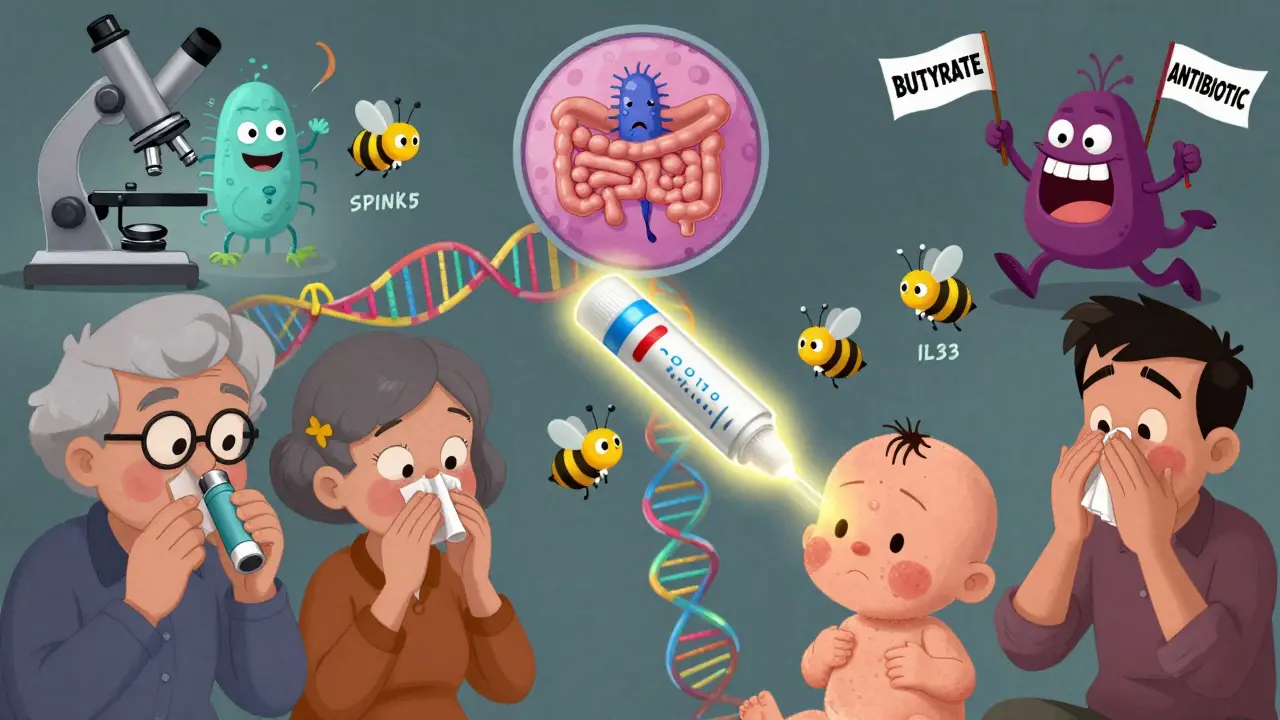
Some kids are born with a genetic disadvantage. Mutations in the filaggrin gene are the most common. Filaggrin is the protein that holds skin cells together like glue. When it’s faulty, skin stays dry, cracks easily, and lets allergens in. About 10-15% of people with eczema carry a filaggrin mutation. But here’s the catch: this mutation doesn’t cause food allergies on its own. It only increases risk when eczema is present. That’s why protecting the skin barrier is so critical-it stops the mutation from triggering the next step. Other genes matter too. Mutations in SPINK5 and corneodesmosin weaken the skin’s outer layer. Polymorphisms in TSLP and IL-33 genes affect immune signaling, making kids more likely to react to allergens in the air or food. These genes don’t act alone-they work together. That’s why eczema, asthma, and hay fever often show up in the same family.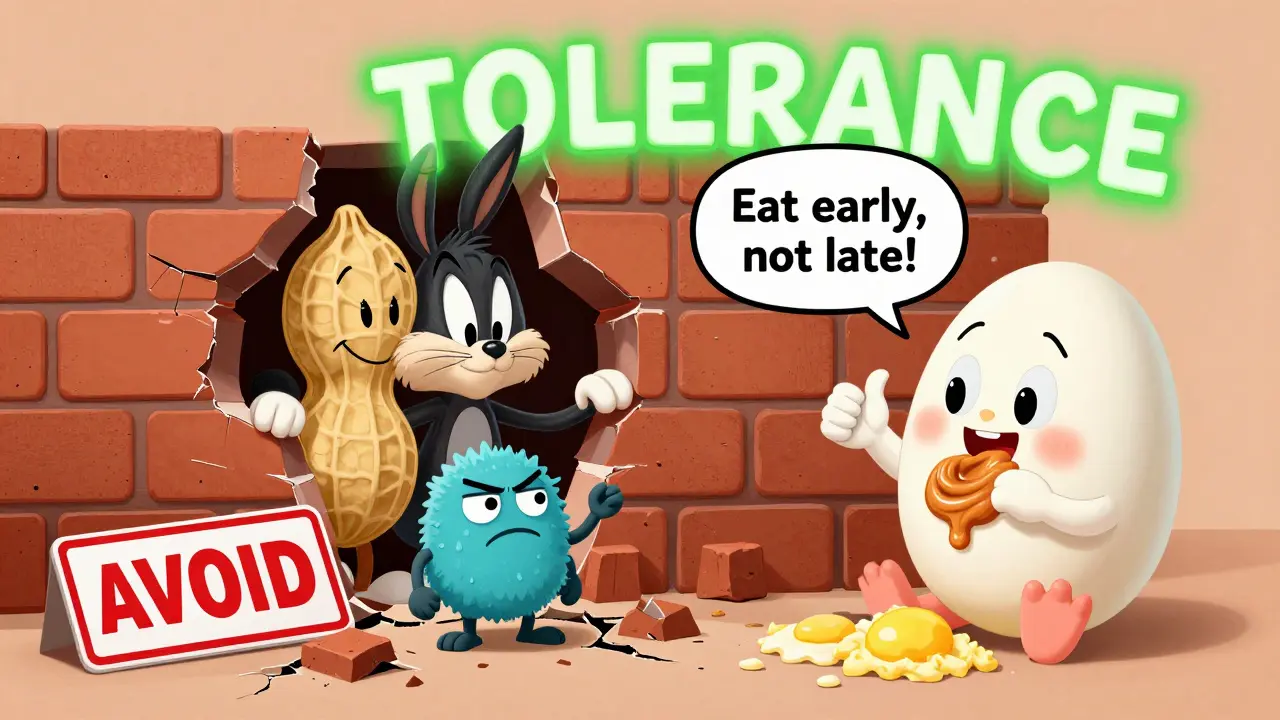
What Skin Barrier Care Actually Looks Like
Skin barrier care isn’t just moisturizing. It’s consistent, daily, and proactive. For babies with eczema-or even just dry skin-here’s what works:- Use fragrance-free, thick ointments like petroleum jelly or ceramide-rich creams. Lotions often have too much water and evaporate fast.
- Apply immediately after bathing, while skin is still damp. This locks in moisture.
- Don’t wait for flare-ups. Apply twice a day, even when skin looks fine.
- Avoid harsh soaps. Use gentle, pH-balanced cleansers-or just water.
- Keep baths short (under 10 minutes) and lukewarm. Hot water strips natural oils.
Gut Health and the Hidden Link
Your baby’s skin isn’t the only barrier. Their gut matters too. Research shows infants who develop allergic sensitization have a different gut microbiome. Specifically, they have less of the bacteria that produce butyrate-a compound that helps train the immune system to stay calm. This doesn’t mean you need to give your baby probiotics right now. The science isn’t there yet. But it does mean avoiding unnecessary antibiotics, especially in the first year. And if you’re breastfeeding, your diet matters. Eating fiber-rich foods supports good bacteria that pass through breast milk. The connection between gut and skin is real. It’s not magic-it’s biology. And it’s another reason why skin care alone isn’t enough. A healthy immune system needs support from the inside, too.When Should You Worry? The 25% Rule
Not every child with eczema needs to be treated like a ticking time bomb. But you should pay attention if:- The eczema is severe, covers large areas, or doesn’t improve with basic moisturizing.
- Your child has a family history of asthma, peanut allergy, or severe hay fever.
- Your baby has other signs of allergy-vomiting after eating eggs, hives after dairy, or wheezing with colds.
What Doesn’t Work (And Why)
A lot of advice out there is outdated-or wrong.- Delaying allergens: Avoiding peanut, egg, or milk doesn’t prevent allergies. It increases risk.
- Using steroid creams only during flares: Waiting until the skin is red and cracked means you’re already behind. Prevention starts before the itch.
- Switching formulas blindly: Unless your baby has a confirmed cow’s milk protein allergy, switching to hydrolyzed formula won’t stop eczema or allergies.
- Over-bathing or using antibacterial soaps: These strip natural oils and make the barrier worse.
The Future: Precision Prevention
Doctors are no longer treating all eczema the same. New tools are emerging to identify which kids are at highest risk:- Genetic testing for filaggrin mutations
- Early skin barrier assessments using non-invasive scans
- Microbiome analysis from stool samples
What You Can Do Today
Start simple:- Apply a thick moisturizer twice daily-morning and night.
- Use gentle, soap-free cleansers.
- If your child has severe eczema, talk to your doctor about introducing peanut and egg before 6 months.
- Keep a symptom diary: note when rashes flare, what foods were eaten, and if breathing changes.
- Don’t panic if your child sneezes in spring. Allergic rhinitis often starts around age three. But if it’s persistent, get it checked.
Is eczema always a sign of future allergies?
No. Most children with eczema won’t develop asthma or food allergies. Only about 25% do-and even then, it’s mostly those with severe eczema. Eczema is a risk factor, not a guarantee.
Can moisturizing prevent food allergies?
It can help. When the skin barrier is strong, allergens can’t sneak in and trigger an immune response. The PreventADALL trial showed daily emollient use reduced eczema by 20-30%, which in turn lowers the chance of developing food allergies. But moisturizing alone isn’t enough-early oral exposure to allergens like peanut is just as important.
Should I avoid giving my baby peanut or eggs if they have eczema?
No. In fact, the opposite is true. For babies with severe eczema, delaying peanut and egg increases allergy risk. The LEAP study showed introducing peanut between 4-11 months reduced peanut allergy by 86%. Talk to your doctor about how and when to safely introduce these foods.
Do probiotics prevent the atopic march?
Not yet proven. While gut bacteria play a role in immune development, current studies haven’t shown that over-the-counter probiotics reliably prevent eczema or allergies. Focus on a healthy diet (especially if breastfeeding) and avoid unnecessary antibiotics instead.
Is the atopic march still a valid concept?
Yes-but not as a strict sequence. The old idea of eczema → food allergy → asthma is outdated. Today, we call it ‘atopic multimorbidity’: multiple allergic conditions can appear together or in different orders. The core idea still holds: early skin barrier damage increases risk. But now we know it’s not inevitable. We can intervene.



anthony epps
December 15, 2025 AT 23:32My kid had eczema bad as a baby. We just kept slathering on vaseline every day after baths. Didn't panic. Didn't change formulas. Just kept it moist. No allergies so far at age 4. Sometimes simple works.
Dylan Smith
December 17, 2025 AT 01:17I used to think moisturizing was just for looks until my daughter broke out in hives after peanut butter. Turns out her skin was cracked from dryness and the allergen slipped in. Now we do ceramide cream twice a day no matter what. It's not glamorous but it's working. No asthma either.
James Rayner
December 17, 2025 AT 03:34There's something deeply poetic about skin being the first line of defense-not just physically, but symbolically. We think of immunity as internal, but it starts at the surface, where the world touches us. The idea that a crack in the barrier can rewrite a child’s future… it’s haunting. And beautiful. We’re not just applying cream-we’re stitching together a fragile, sacred boundary between the self and the world. I cried reading this. Not because I’m sad, but because I finally understood what I’ve been doing all these months.
Souhardya Paul
December 18, 2025 AT 08:27For anyone new to this-don’t overcomplicate it. Moisturize. Introduce allergens early. Avoid harsh soaps. That’s the core. The science is cool, but the action is simple. I’m a nurse and I’ve seen parents stress over every ingredient, every brand, every probiotic. You don’t need all that. Just be consistent. Your kid doesn’t need perfect-they need predictable. And love. Always love.
Josias Ariel Mahlangu
December 19, 2025 AT 11:39They want you to believe this ‘atopic march’ nonsense so they can sell you creams and tests. Back in my day, we just washed with soap and let kids play in dirt. No allergies. Now every kid’s on a cream regimen and gets tested for everything. This is corporate medicine selling fear to make money.
Arun ana
December 21, 2025 AT 10:47My cousin in India had eczema since birth. Grandma used coconut oil and turmeric paste. No fancy creams. No doctor visits. Kid grew up fine. No allergies. Maybe we’re overmedicalizing normal skin? 🤔
Dave Alponvyr
December 23, 2025 AT 01:36So let me get this straight… we’re supposed to rub petroleum on a baby’s face and then feed them peanut butter to prevent allergies? Next you’ll tell me to give them a shot of whiskey for a cold.
Cassandra Collins
December 23, 2025 AT 03:46Did you know the FDA is hiding the truth? The real cause of eczema is 5G radiation + glyphosate in baby formula. They don’t want you to know that moisturizers are just a distraction so Big Pharma can sell asthma inhalers later. My cousin’s baby got better after she switched to organic breastmilk and wrapped the baby in aluminum foil at night. It’s not science-it’s suppression.
Elizabeth Bauman
December 24, 2025 AT 23:50I love how this article treats Western medicine like the only truth. In my country, we’ve been using traditional herbal baths for generations. Why are we suddenly listening to American studies? Our ancestors knew how to heal skin without ceramides and lab tests. This is cultural imperialism disguised as science.
Tiffany Machelski
December 25, 2025 AT 09:13i just started using the cera ve cream after reading this and my son’s skin is already less red… i think i was using too much soap before? not sure but this helped. thanks for sharing!!
Andrew Sychev
December 25, 2025 AT 10:42My daughter had eczema at 3 months. We did everything right. Moisturized. Introduced peanut at 5 months. Took her to three specialists. She still got asthma by age 2. So what’s the point? We did everything they said. And it still happened. This isn’t prevention-it’s guilt. They make you feel like a bad parent if your kid still gets sick. I’m done.
Dan Padgett
December 25, 2025 AT 20:42Back home in Nigeria, we say skin is the mirror of the soul. When a baby’s skin cracks, it’s not just a physical thing-it’s a sign the family’s rhythm is off. Maybe too much stress. Maybe too much processed food. Maybe the baby needs more holding, more singing, more quiet. We don’t just slap cream on it. We hold them. We sing. We feed the mother yams and bitter leaf. The skin heals because the spirit is soothed. Science can measure ceramides, but can it measure love?