What Is Gestational Diabetes?
Gestational diabetes, or GDM, happens when your body can’t make enough insulin during pregnancy to handle the extra sugar in your blood. It usually shows up between weeks 24 and 28, when hormones from the placenta start blocking insulin. Your pancreas has to work harder-sometimes up to three times harder-to keep your blood sugar steady. When it can’t keep up, sugar builds up, and that’s gestational diabetes.
This isn’t something you had before pregnancy. It’s temporary, but it needs attention. Left unmanaged, it can lead to a baby weighing over 9 pounds, difficulty during delivery, low blood sugar in the newborn, or even preeclampsia for the mother. The good news? With the right plan, most women with GDM have perfectly healthy pregnancies and babies.
How Do You Know If You Have It?
Most women get screened between 24 and 28 weeks with a simple glucose challenge test. You drink a sugary solution, and an hour later, your blood is drawn. If your level is above 140 mg/dL, you’ll need a longer test-the oral glucose tolerance test (OGTT). This one takes three hours and involves four blood draws after drinking a stronger sugar solution.
Some clinics use a lower cutoff-130 mg/dL-to catch more cases early. Diagnosis comes if two or more of those four readings are too high. You might be tested earlier if you’ve had GDM before, are overweight, have a family history of diabetes, or are over 35.
Don’t wait for symptoms. Most women feel fine. No excessive thirst, no frequent urination-just a quiet rise in blood sugar that only a test can reveal.
What Are the Blood Sugar Targets?
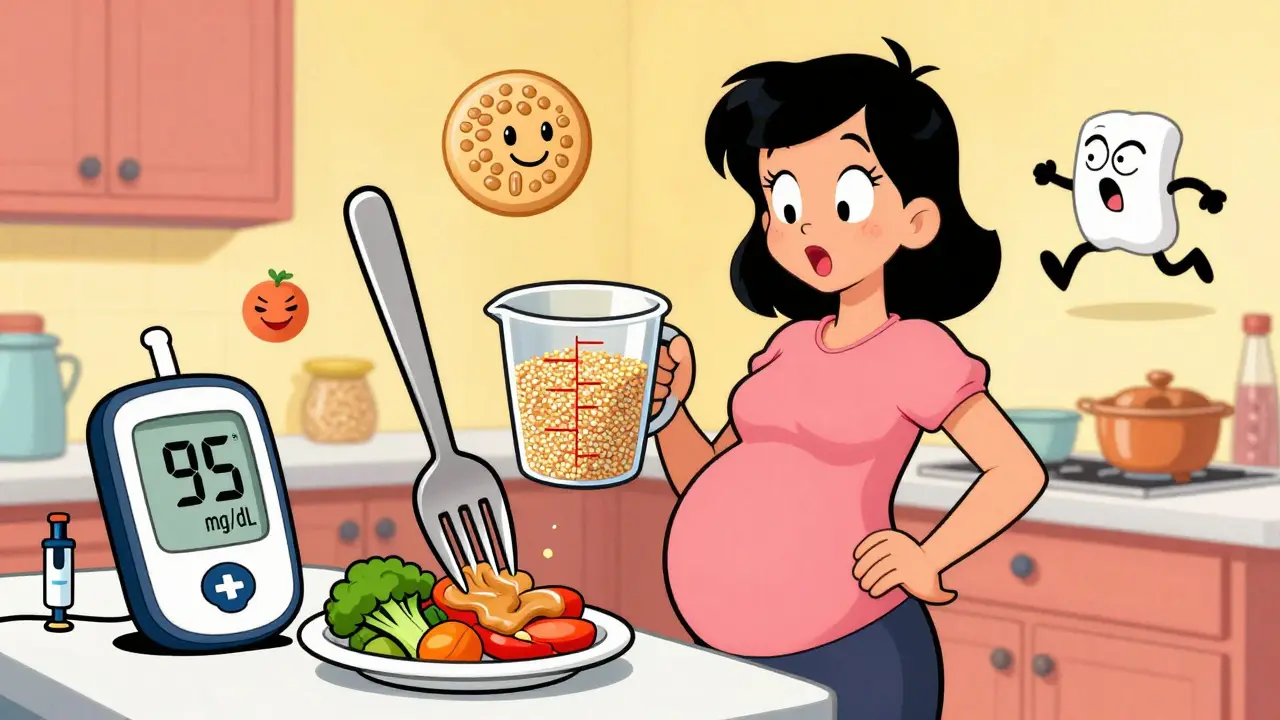
If you’re diagnosed, your goal is simple: keep your numbers as close to a non-diabetic pregnant woman’s as possible. Here’s what your care team will aim for:
- Fasting or before meals: under 95 mg/dL
- One hour after eating: under 140 mg/dL
- Two hours after eating: under 120 mg/dL
These aren’t suggestions-they’re the targets backed by research from the American Diabetes Association. Staying within them cuts your baby’s risk of being too large, needing NICU care, or having low blood sugar after birth.
Many women check their blood sugar four to six times a day: first thing in the morning, and then one to two hours after each meal. Keeping a log-what you ate, when you ate, and your numbers-helps spot patterns. Is your sugar high after breakfast? Maybe your morning toast is too much. Is it high at bedtime? You might need a small snack with protein before sleep.
Diet: What to Eat and What to Avoid
Diet is the first and most powerful tool. About 80% of women manage GDM with food alone.
Carbohydrates are your biggest challenge-but they’re not the enemy. You still need them. The trick is type, amount, and timing.
- Choose complex carbs: whole grains, oats, quinoa, beans, lentils, sweet potatoes. Avoid white bread, white rice, pastries, and sugary cereals.
- Limit carbs to 17-19 servings per day (1 serving = 15 grams of carbs). That’s about 45 grams per meal and 15-30 grams per snack.
- Pair every carb with protein or fat: an apple with peanut butter, yogurt with nuts, or cheese with whole grain crackers. This slows sugar absorption and keeps your numbers steady.
Try the protein-first method: eat your meat, eggs, or tofu first, then vegetables, then carbs. One study found this lowered post-meal spikes by 25-40 mg/dL.
Portion control matters. One cup of cooked rice or pasta? That’s one meal’s worth. Two slices of whole grain bread? That’s your carb allotment for breakfast. Use measuring cups at first. Guessing leads to spikes.
Don’t skip meals. Eat three small meals and two to three snacks daily. Going too long without food can cause your liver to dump sugar into your blood, raising your fasting levels.
Exercise: The Hidden Secret
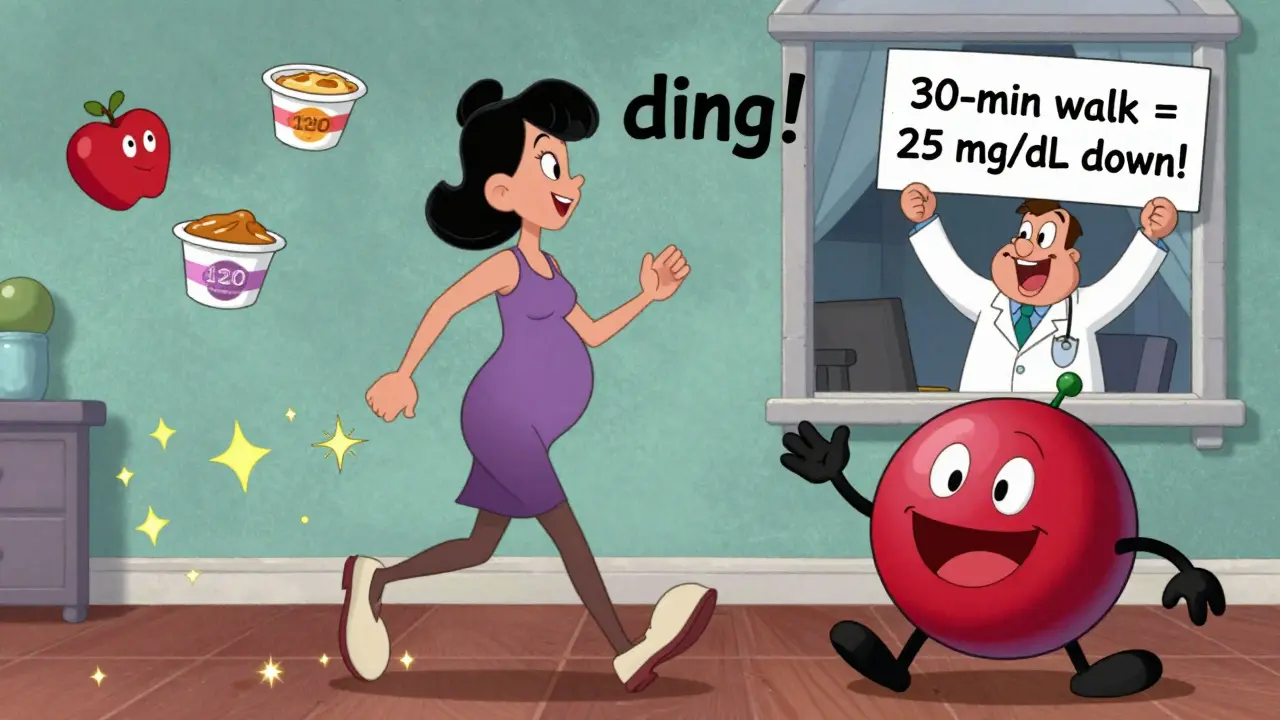
Physical activity is like a natural insulin. It helps your muscles pull sugar out of your blood-without needing extra insulin.
Walk for 30 minutes, five days a week. Brisk walking after meals is especially powerful. A 15- to 30-minute walk after dinner can drop your blood sugar by 20-30 mg/dL. Swimming and prenatal yoga are also great.
Don’t wait until you feel like it. Do it right after eating. Set a reminder on your phone. If you can’t get outside, walk in place while watching TV. Movement doesn’t have to be intense-just consistent.
One woman on Reddit shared that her fasting numbers dropped 15-25 mg/dL just by walking every morning before breakfast. That’s the kind of change that makes a difference.
When You Need More Than Diet and Exercise
Even with perfect food and daily walks, about 15-30% of women still need medication. That doesn’t mean you failed. Your body just needed a little extra help.
Insulin is the most common treatment. It’s safe for your baby. Many women worry about needles, but the pens are small, and the needles are tiny. Most get used to them in a few days. Your provider will teach you how to inject and when.
Metformin is sometimes used, especially if insulin isn’t available or preferred. But studies show about 30% of women on metformin still end up needing insulin anyway. It’s not a magic fix.
Some women use continuous glucose monitors (CGMs). These are small sensors worn on the arm that track sugar levels 24/7. They’re not standard yet, but they’re growing in use. One study showed a 39% drop in large babies when women used CGMs instead of finger sticks. If your provider offers it, ask about it.
What Happens After the Baby Is Born?
Most women’s blood sugar returns to normal within days of delivery. But that doesn’t mean you’re out of the woods.
Between 6 and 12 weeks after birth, you’ll get a 75-gram oral glucose tolerance test. If your fasting level is above 126 mg/dL or your 2-hour level is above 200 mg/dL, you have Type 2 diabetes. If it’s high but not there yet, you have prediabetes.
Here’s the hard truth: 50% of women with GDM will develop Type 2 diabetes within 10 years. But you can stop that.
Studies show that losing 5-7% of your body weight in the year after birth-through diet and exercise-cuts your risk by 58%. That’s not about being thin. It’s about staying active and eating well, even after the baby arrives.
Get screened every two years after that. And if you get pregnant again, you’ll be tested early-because once you’ve had GDM, you’re much more likely to get it again.

Emotional Support Matters Too
Getting diagnosed with gestational diabetes can feel overwhelming. One in two women say they felt anxious or guilty at first. You might worry about injections, food restrictions, or your baby’s health.
You’re not alone. Support groups-online or in person-help. Reddit’s r/GestationalDiabetes has thousands of women sharing tips, recipes, and reassurance. DiabetesSisters offers free coaching and meal plans.
Don’t let shame silence you. Ask your provider for a referral to a certified diabetes care and education specialist (CDCES). They’re trained to help you understand your numbers, adjust your meals, and cope with stress. Most clinics offer weekly check-ins for the first month. Use them.
What If You Don’t Manage It?
Ignoring GDM doesn’t mean you’re a bad mom. But it does raise real risks:
- Your baby could grow too large, making delivery harder and increasing the chance of a C-section or shoulder injury.
- Your baby might be born with low blood sugar and need IV glucose in the NICU.
- You’re more likely to develop high blood pressure or preeclampsia.
- Long-term, your child is more likely to become overweight or develop Type 2 diabetes later in life.
And the numbers don’t lie: women who check their blood sugar less than four times a day have more than double the risk of NICU admission for their babies.
This isn’t about fear. It’s about control. You’re not powerless. You have tools. You have choices. You have time.
Key Takeaways
- Gestational diabetes is common, treatable, and doesn’t mean you did anything wrong.
- Stick to your blood sugar targets: fasting under 95, 1-hour under 140, 2-hour under 120.
- Carbs are okay-just choose whole grains, control portions, and always pair with protein or fat.
- Walk after meals. It’s simple, free, and powerful.
- Medication isn’t failure. Insulin is safe and effective.
- Postpartum testing and lifestyle changes cut your future diabetes risk by more than half.
- Ask for help. You don’t have to do this alone.




Guillaume VanderEst
December 20, 2025 AT 02:36Marsha Jentzsch
December 21, 2025 AT 07:02Erica Vest
December 22, 2025 AT 03:19Chris Davidson
December 24, 2025 AT 01:59Alisa Silvia Bila
December 24, 2025 AT 15:40Danielle Stewart
December 26, 2025 AT 00:56Dominic Suyo
December 27, 2025 AT 07:33Aadil Munshi
December 29, 2025 AT 04:14Kinnaird Lynsey
December 31, 2025 AT 01:05Frank Drewery
January 1, 2026 AT 17:52Kevin Motta Top
January 3, 2026 AT 04:53James Stearns
January 3, 2026 AT 09:25Carolyn Benson
January 4, 2026 AT 04:35Adrienne Dagg
January 5, 2026 AT 15:07Aadil Munshi
January 6, 2026 AT 05:06