RCC Angiogenesis Inhibitor Selector
Recommended Treatment Options
Drug Information
Sunitinib
Target: VEGFR-1/2/3, PDGFR
Dose: 50 mg daily 4 weeks on/2 weeks off
ORR: 31%
Pazopanib
Target: VEGFR-1/2/3, PDGFR, c-KIT
Dose: 800 mg once daily
ORR: 28%
Axitinib
Target: VEGFR-1/2/3
Dose: 5 mg twice daily
ORR: 23%
Cabozantinib
Target: MET, VEGFR-2, AXL
Dose: 60 mg once daily
ORR: 21%
Bevacizumab
Target: VEGF-A
Dose: 10 mg/kg IV every 2 weeks
ORR: 15%
When you hear the term angiogenesis inhibitors, you might picture a high‑tech weapon aimed at cancer’s lifeline. In reality, these drugs are part of a standard playbook for battling renal cell carcinoma (RCC), the most common kidney cancer type. This guide breaks down how they work, which agents are front‑line, and what patients and clinicians should watch for during therapy.
Key Takeaways
- Angiogenesis inhibitors block the VEGF pathway, cutting off the blood supply tumors need to grow.
- First‑line RCC regimens now pair an inhibitor with an immune checkpoint blocker for higher response rates.
- Side‑effects like hypertension and hand‑foot syndrome can be managed with dose tweaks and supportive care.
- Biomarkers such as VHL mutations help predict who benefits most.
- Staying current with NCCN guidelines ensures patients receive the most effective, evidence‑based combinations.
What Is Renal Cell Carcinoma?
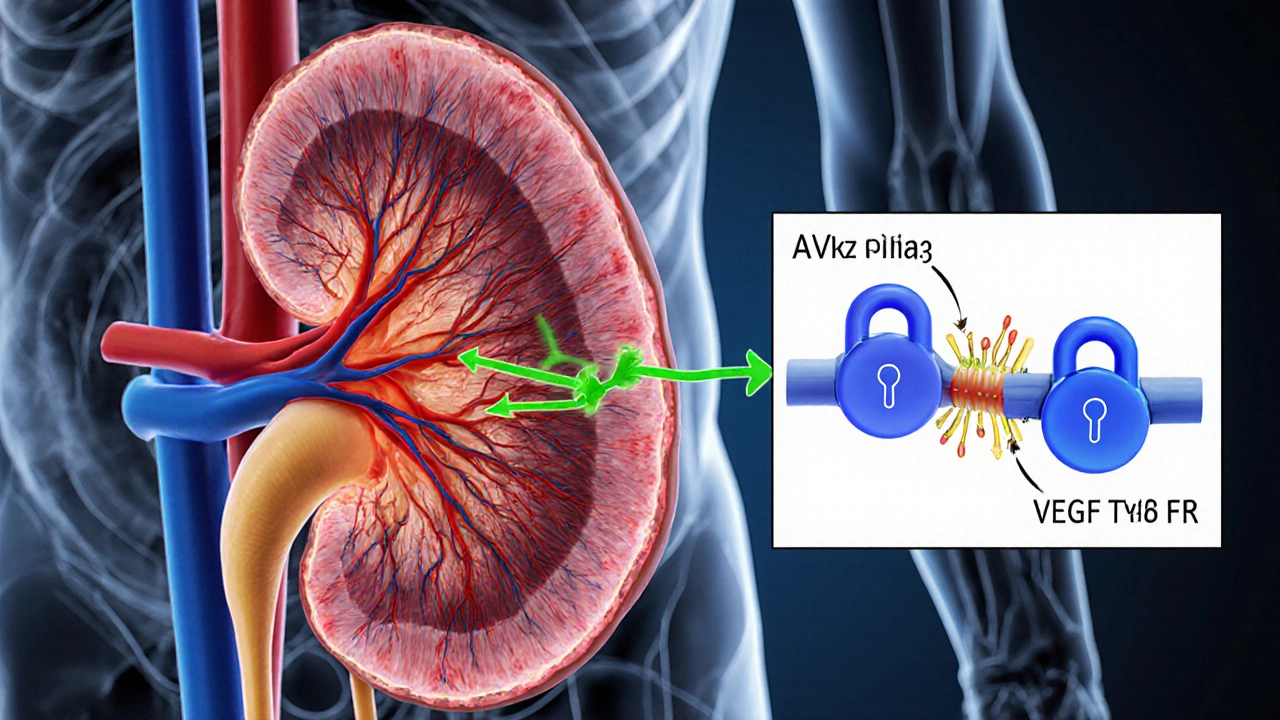
Renal Cell Carcinoma is a malignant tumor that originates in the renal tubular epithelium of the kidney. It accounts for about 90% of kidney cancers and often presents with hematuria, flank pain, or an incidental mass on imaging. The disease is notorious for being highly vascular, which is why cutting off its blood supply can make a huge difference.
Why Target Angiogenesis?
Kidney tumors overproduce vascular endothelial growth factor (VEGF) because many carry mutations in the VHL gene. When VHL is lost, hypoxia‑inducible factor (HIF) builds up, driving VEGF production and new vessel growth. By interfering with this cascade, Angiogenesis Inhibitor a class of drugs that prevents new blood vessel formation, thereby starving tumors of nutrients effectively starves the tumor.
Major Angiogenesis Inhibitors Used in RCC
Below is a quick look at the most widely prescribed agents, their primary targets, and key clinical facts.
| Drug | Primary Target | Typical Dose | Objective Response Rate (ORR) | Common Side Effects |
|---|---|---|---|---|
| Sunitinib | VEGFR‑1/2/3, PDGFR | 50mg daily4weeks on/2weeks off | 31% | Hypertension, fatigue, hand‑foot syndrome |
| Pazopanib | VEGFR‑1/2/3, PDGFR, c‑KIT | 800mg once daily | 28% | Elevated liver enzymes, nausea, hypertension |
| Axitinib | VEGFR‑1/2/3 | 5mg twice daily (adjustable) | 23% | Diarrhoea, hypertension, fatigue |
| Cabozantinib | MET, VEGFR‑2, AXL | 60mg once daily | 21% | Palmar‑plantar erythrodysesthesia, hypertension, diarrhoea |
| Bevacizumab (in combo with interferon‑α) | VEGF‑A | 10mg/kg IV every 2weeks | 15% | Proteinuria, bleeding, hypertension |

How These Drugs Fit Into Modern RCC Regimens
Guidelines from the NCCN and ESMO now recommend combining an angiogenesis inhibitor with an immune checkpoint inhibitor (ICI) such as pembrolizumab or nivolumab. The rationale is simple: while the TKI chops off the tumor’s blood supply, the ICI re‑activates T‑cells to attack the cancer.
Typical first‑line combos include:
- Sunitinib+pembrolizumab
- Axitinib+pembrolizumab (KEYNOTE‑426 trial showed 59% ORR)
- Cabozantinib+nivolumab (CheckMate‑9ER reported 55% ORR)
These mixtures have pushed median overall survival beyond 4years in many patients, a dramatic improvement over the era of cytokine therapy alone.
Managing Side‑Effects: Practical Tips
Angiogenesis inhibitors are effective, but they come with a predictable side‑effect profile. Here’s what clinicians and patients can do:
- Hypertension: Check blood pressure weekly during the first two months. Start an ACE inhibitor or calcium‑channel blocker early; many patients need two agents.
- Hand‑Foot Syndrome (palmar‑plantar erythrodysesthesia): Apply urea‑based creams twice daily, avoid tight shoes, and keep skin cool.
- Liver Enzyme Elevation: Monitor ALT/AST every 2weeks for the first 8weeks. If levels exceed three times upper limit, dose‑reduce or pause treatment.
- Diarrhoea: Use loperamide at the first sign; stay hydrated and consider a low‑residue diet.
- Proteinuria: Spot urine protein quarterly; hold therapy if >2g/24h.
Open communication is key-most patients experience better quality of life when side‑effects are addressed proactively.
Predicting Who Will Benefit: Biomarkers and Genetics
While everyone with advanced RCC gets a TKI‑based regimen, researchers are hunting biomarkers to personalize therapy further. The most promising signals include:
- VHL mutation status: Loss of VHL drives VEGF; patients with clear‑cell histology (most RCC cases) tend to respond well.
- PD‑L1 expression: Higher levels may predict a better response to ICI‑TKI combos.
- Gene expression signatures: Ongoing trials evaluate angiogenesis‑related gene panels to tailor the choice of TKI.
At present, NCCN guidelines recommend using clinical risk models (e.g., IMDC criteria) rather than any single biomarker to decide between monotherapy and combination therapy.
Future Directions: Next‑Generation Inhibitors
Research labs are designing drugs that hit multiple pathways simultaneously-think VEGF, MET, and AXL in one molecule. Early‑phase trials of agents like lenvatinib‑cabozantinib hybrids show ORRs approaching 40% in heavily pre‑treated patients.
Beyond small‑molecule TKIs, novel approaches such as antibody‑drug conjugates targeting VEGF‑R2 are entering phaseII studies. If these pans out, the treatment landscape may shift again, offering more precise-and potentially less toxic-options.
Putting It All Together: A Practical Decision Tree
When a physician faces a newly diagnosed metastatic RCC patient, the following flow can help decide the right regimen:
- Assess IMDC risk (favorable, intermediate, poor).
- If favorable risk and patient prefers oral therapy, start sunitinib or pazopanib monotherapy.
- If intermediate or poor risk, move straight to an ICI‑TKI combo (axitinib+pembrolizumab or cabozantinib+nivolumab).
- Monitor blood pressure, liver enzymes, and skin health closely during the first 8weeks.
- At progression, consider switching to a different TKI or enrolling in a clinical trial of a next‑generation inhibitor.
This roadmap keeps treatment evidence‑based while staying flexible for individual patient needs.
Frequently Asked Questions
What makes angiogenesis inhibitors effective against kidney cancer?
Kidney tumors rely heavily on new blood vessels formed through the VEGF pathway. By blocking VEGF receptors, angiogenesis inhibitors cut off the tumor’s nutrient supply, slowing growth and sometimes shrinking the mass.
Are oral TKIs or IV drugs better for RCC?
Both have a place. Oral TKIs like sunitinib and pazopanib are convenient and have proven efficacy. IV agents such as bevacizumab are usually used in combination with other therapies. Choice depends on patient preference, comorbidities, and risk profile.
How soon should side‑effects be reported?
Patients should report new symptoms within the first two weeks of starting therapy. Early intervention can prevent dose reductions later on.
Can I combine more than one angiogenesis inhibitor?
Combining two VEGF‑targeting TKIs has not shown added benefit and increases toxicity. Current practice pairs one TKI with an immune checkpoint inhibitor instead.
What are the latest NCCN guideline updates for RCC?
The 2024 NCCN update recommends first‑line ICI‑TKI combos for most patients with intermediate or poor risk disease, while allowing TKI monotherapy for favorable risk patients who prefer oral treatment.




Megan Lallier-Barron
October 4, 2025 AT 01:33Isn't it curious how we treat angiogenesis inhibitors as if they're miracle weapons, while they're really just molecular keys that lock a tumor's blood supply? 🤔 The history of RCC therapy shows a pattern of hype followed by sober reality. Still, the rise of combination regimens feels like a philosophical paradox: more complexity for a clearer outcome.
Kelly Larivee
October 9, 2025 AT 04:13The guide does a solid job breaking down the drug options.
Emma Rauschkolb
October 14, 2025 AT 06:53Delving into the VEGF axis unveils a cascade of downstream signaling that intertwines with hypoxia‑inducible factors, creating a labyrinthine network of pro‑angiogenic stimuli. The pharmacodynamic profile of sunitinib, for instance, exhibits a multi‑targeted kinase inhibition that transcends mere VEGFR blockade, thereby influencing PDGFR and FLT3 pathways. 📈 Yet, the clinical translation often battles with pharmacokinetic variability and emergent resistance mechanisms that are as capricious as they are relentless. One cannot ignore the ethological impact of hypertension and hand‑foot syndrome on patient adherence – the latter being a dermatologic manifestation that feels almost poetic in its distribution across acral surfaces. 😅
Kaushik Kumar
October 19, 2025 AT 09:33First‑line therapy for metastatic RCC has dramatically evolved over the past decade! The integration of immune checkpoint inhibitors with VEGF tyrosine‑kinase inhibitors creates a synergistic assault on tumor vasculature and immune evasion! Clinical trials such as KEYNOTE‑426 and CheckMate‑9ER have demonstrated overall survival benefits that were previously unimaginable! Patients with intermediate or poor IMDC risk now have median survivals exceeding four years, a landmark achievement! The therapeutic landscape emphasizes personalized risk stratification, guiding the choice between monotherapy and combination regimens! Oral agents like sunitinib and pazopanib provide convenience but demand vigilant monitoring of blood pressure and hepatic function! Combination regimens, for example axitinib plus pembrolizumab, amplify response rates while introducing a new spectrum of immune‑related adverse events! Dose adjustments remain a critical tool, allowing clinicians to balance efficacy with tolerability! Hypertension, a class effect of VEGF inhibition, must be managed proactively with antihypertensives to prevent cardiovascular complications! Hand‑foot syndrome requires dose reductions and supportive skin care to maintain quality of life! Diarrhea, another common toxicity, can be mitigated with antidiarrheal agents and dietary modifications! Regular laboratory assessments, including liver enzymes and proteinuria screening, are indispensable for early detection of organ‑specific toxicity! The emergence of biomarker‑driven approaches, such as PD‑L1 expression and VHL mutational status, hints at future refinement of therapy selection! Ongoing phase III studies are evaluating next‑generation multi‑targeted agents that concurrently inhibit MET, AXL, and VEGFR pathways! Ultimately, the goal remains clear: to extend survival while preserving patient dignity and functional capacity!
Mara Mara
October 24, 2025 AT 12:13Indeed, the progress is remarkable-particularly for American patients who benefit from cutting‑edge clinical trials! The meticulous dose titration you described showcases the precision medicine ethos that the United States has championed for years! Let’s not forget that access to these therapies also hinges on robust healthcare infrastructure and insurance support, which remain critical pillars of our national success.
Jennifer Ferrara
October 29, 2025 AT 13:53When one contemples the evolution of renal cell carcinoma management, the juxtaposition of targeted therapy and immunotherapy emerges as a seminal paradigm shift. The evidencce from landmark studies underscores a tangible improvement in overall survival, albeit with nuanced considerations regarding toxicity profiles. Moreover, the integration of biomarker insights such as VHL muta tion delineates a more refined stratification of patients. It is imperitive that clinicians remain apprised of the latest NCCN guIdelines to engender optimal outcomes. In sum, the confluence of angiogenesis inhibition and checkpoint blockade heralds a new epoch in oncologic care.
Terry Moreland
November 3, 2025 AT 16:33That’s a great summary-thanks for laying it out so clearly! It really helps patients and families understand why combination therapy can be worth the extra monitoring. Keep the simple explanations coming; they make a big difference.
Abdul Adeeb
November 8, 2025 AT 19:13The regulatory framework in the United States mandates rigorous phase III evaluation before approval of any angiogenesis inhibitor. Consequently, clinicians can rely on robust safety and efficacy data when prescribing these agents.
Abhishek Vernekar
November 13, 2025 AT 21:53While the data is indeed reassuring, the human element of therapy cannot be overlooked. The emotional burden of side‑effects often shadows the clinical triumphs, creating a dichotomy that patients must navigate. Empathy, therefore, should accompany every prescription, ensuring that support structures are in place. Ultimately, the goal is to merge scientific rigor with compassionate care.
Val Vaden
November 19, 2025 AT 00:33Looks like another fluff piece 😒