Thyroid-Ischemia Risk Calculator
Thyroid-Ischemia Risk Assessment
This tool estimates your risk of ischemic complications based on thyroid function and key risk factors. The calculation is based on clinical guidelines and research from 2023-2024.
Your Risk Assessment
Quick Takeaways
- Both low and high thyroid hormone levels can trigger or worsen tissue ischemia.
- Ischemia‑driven oxidative stress often aggravates autoimmune thyroid disease.
- Managing blood flow, cholesterol, and thyroid hormone balance cuts the risk of heart attacks and strokes.
- Regular screening for thyroid function in patients with chronic vascular disease is a cost‑effective preventive step.
When blood can’t reach a tissue fast enough, that tissue suffers from ischemia. At the same time, the thyroid gland-your body’s metabolic thermostat-can go off‑track, leading to disorders like hypothyroidism or hyperthyroidism. What’s the hidden thread that ties these two seemingly different problems together? Recent research shows that poor blood flow and thyroid hormone imbalances feed each other, creating a vicious cycle that raises the odds of heart disease, stroke, and even chronic fatigue.
Below you’ll find a plain‑language breakdown of the biology, the key risk factors, practical steps for clinicians and patients, and answers to the most common questions.
What Is Ischemia?
Ischemia is a condition where blood flow to a tissue is insufficient to meet its oxygen and nutrient demands. This can happen suddenly, as in a heart attack, or develop slowly, as in peripheral artery disease. The hallmark signs-pain, pallor, tingling-often signal that cells are switching from aerobic to anaerobic metabolism, producing lactic acid and reactive oxygen species (ROS).
Understanding Thyroid Disorders
Thyroid disorders comprise a spectrum of conditions that affect how the thyroid gland produces two main hormones: thyroxine (T4) and triiodothyronine (T3). The two most common clinical presentations are:
- Hypothyroidism - the gland under‑produces hormones, slowing metabolism.
- Hyperthyroidism - excess hormone output, speeding up metabolism.
Autoimmune thyroiditis (Hashimoto’s disease) and Graves’ disease are the leading causes of these hormonal imbalances. Both involve the immune system producing antibodies that either destroy thyroid tissue or stimulate it.
How Thyroid Hormones Influence Blood Vessels
Thyroid hormones are more than just energy regulators; they directly affect the cardiovascular system:
- Vasodilation: T3 promotes nitric oxide (NO) production in endothelial cells, relaxing blood vessels and improving flow.
- Heart contractility: Both T3 and T4 increase heart rate and stroke volume, affecting cardiac output.
- Lipid metabolism: Adequate thyroid function helps keep LDL cholesterol low, reducing atherosclerotic plaque buildup.
When hormone levels veer off the normal range, these mechanisms falter.
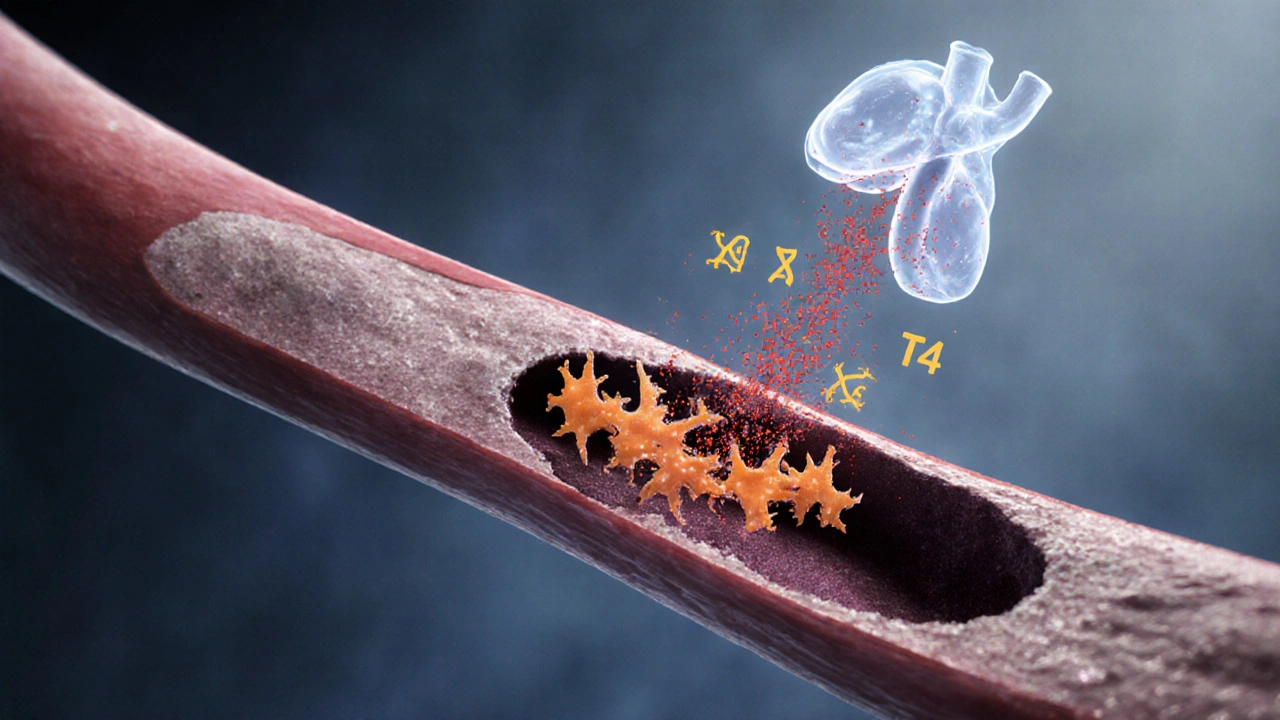
The Biological Loop: From Thyroid Imbalance to Ischemia
Let’s follow the chain of events when hypothyroidism takes hold:
- Low T3/T4 reduces nitric oxide synthesis → endothelial dysfunction develops.
- Endothelial dysfunction raises vascular resistance, limiting blood supply to muscles, brain, and heart.
- Reduced perfusion causes localized ischemia, which triggers oxidative stress and inflammation.
- Oxidative stress damages thyroid follicular cells, potentially worsening autoimmune activity and deepening hypothyroidism.
Hyperthyroidism can flip the script. Excess hormones increase cardiac output and heart rate, but they also raise blood pressure and promote a hypercoagulable state. The net effect is increased shear stress on vessel walls, accelerating atherosclerosis and setting the stage for ischemic events.
Key Clinical Links Between Ischemia and Thyroid Disease
| Thyroid State | Vascular Impact | Typical Ischemic Risk |
|---|---|---|
| Hypothyroidism | Reduced NO, higher LDL, slowed heart rate | Coronary artery disease, peripheral arterial disease |
| Hyperthyroidism | Elevated cardiac output, increased shear stress, hypercoagulability | Arrhythmia‑related emboli, myocardial ischemia |
| Euthyroid (normal) | Balanced endothelial function | Baseline population risk |
Risk Factors That Amplify the Connection
Not everyone with a thyroid issue will develop ischemia, but certain co‑variables tip the scales:
- Age: Vascular elasticity naturally declines after 50, magnifying hormone‑related effects.
- Gender: Women are more prone to autoimmune thyroid disease, while men have higher baseline cardiovascular risk.
- Smoking: Impairs NO production, worsening both endothelial dysfunction and thyroid autoimmunity.
- Metabolic syndrome: High triglycerides and insulin resistance synergize with low thyroid function to accelerate plaque formation.
Diagnostic Tips for Clinicians
When a patient presents with chest pain, leg claudication, or unexplained fatigue, consider a two‑pronged assessment:
- Vascular evaluation: Ankle‑brachial index (ABI), coronary calcium scoring, or stress echocardiography to detect ischemia.
- Thyroid panel: TSH, free T4, free T3, plus thyroid antibodies (anti‑TPO, TRAb) if autoimmune disease is suspected.
Studies from 2023‑2024 show that patients with TSH >10µIU/mL have a 1.8‑fold higher odds of having a positive ABI (<0.9), indicating peripheral arterial disease.

Management Strategies That Hit Both Targets
Therapies that improve blood flow often help normalize thyroid function, and vice versa.
1. Optimize Thyroid Hormone Levels
- For hypothyroidism, levothyroxine titration to keep TSH between 0.5‑2.5µIU/mL reduces LDL by ~10% and improves endothelial function markers.
- In hyperthyroidism, antithyroid drugs (methimazole) or definitive therapy (radioiodine) lower heart rate and decrease atrial fibrillation risk, cutting embolic stroke chances.
2. Enhance Endothelial Health
- Exercise: 150minutes of moderate aerobic activity weekly boosts NO availability and can lower TSH by ~0.5µIU/mL in subclinical hypothyroid patients.
- Diet: Mediterranean‑style meals rich in omega‑3 fatty acids improve lipid profiles and support thyroid hormone conversion (T4 → T3).
- Statins: Beyond cholesterol lowering, statins have pleiotropic effects that stabilize plaque and modestly improve thyroid peroxidase antibody levels.
3. Control Co‑morbidities
- Manage hypertension with ACE inhibitors, which also enhance endothelial resilience.
- Address insulin resistance through metformin or lifestyle changes; metformin has been shown to reduce TSH in some hypothyroid patients.
Red Flags: When to Seek Immediate Care
If a patient with known thyroid disease experiences sudden chest pressure, shortness of breath, or limb numbness, treat it as a potential acute ischemic event. Prompt ECG and cardiac enzymes, alongside urgent thyroid function reassessment, are critical.
Future Directions in Research
Emerging data from the 2025 International Thyroid‑Cardio Conference highlight two promising avenues:
- Selective T3 analogs: Compounds that enhance vascular NO without triggering tachyarrhythmias are in Phase II trials.
- Micro‑RNA therapeutics: Targeting miR‑210, which is up‑regulated during both ischemia and autoimmune thyroiditis, may break the feedback loop.
These innovations could soon give clinicians tools that address the root of the ischemia‑thyroid connection rather than just managing symptoms.
Frequently Asked Questions
Can low thyroid function cause a heart attack?
Yes. Untreated hypothyroidism raises LDL cholesterol and reduces nitric oxide, both of which accelerate atherosclerosis. Over time, plaque can rupture, leading to myocardial infarction. Keeping TSH within the normal range cuts this risk substantially.
Do thyroid medications improve circulation?
When the dose is right, levothyroxine restores normal metabolic rates, which helps endothelial cells produce more nitric oxide. Patients often report less cold intolerance and better exercise tolerance, indicating better blood flow.
Is there a screening protocol for thyroid problems in patients with peripheral artery disease?
Guidelines suggest a baseline TSH test for anyone diagnosed with PAD. If TSH is abnormal, follow up with free T4 and thyroid antibody panels. Early detection lets clinicians adjust hormone therapy before severe ischemia develops.
Can hyperthyroidism cause stroke?
Yes, especially if atrial fibrillation develops. Excess thyroid hormones increase cardiac output and provoke irregular rhythms, which can launch clots that travel to the brain. Controlling thyroid hormone levels reduces the arrhythmia burden and stroke risk.
What lifestyle changes help both thyroid health and vascular perfusion?
Regular aerobic exercise, a Mediterranean diet rich in fish, nuts, and olive oil, quitting smoking, and maintaining a healthy weight all improve lipid profiles, reduce inflammation, and support proper thyroid hormone conversion.



Mita Son
October 14, 2025 AT 20:04Wow, the link between ischemia and thyroid issues is like a hidden trap waiting to bite you. If your TSH is sky‑high, you’re practically waving a red flag for blood‑flow problems. Keep an eye on those numbers, girl!
ariel javier
October 15, 2025 AT 12:44Your risk calculator is fundamentally flawed.
Bryan L
October 16, 2025 AT 04:00I totally get how overwhelming these scores can feel, especially when you’re juggling meds 😔.
Remember, a high score isn’t a death sentence-it’s a cue to tweak lifestyle and maybe talk to your endocrinologist.
Small steps make big differences!
joseph rozwood
October 16, 2025 AT 21:14Honestly, this shiny widget looks like a gimmick slapped onto a centuries‑old endocrine debate. The algorithms feel half‑baked, as if someone threw in arbitrary points for smoking and age without proper citation. It’s more flash than substance.
Richard Walker
October 17, 2025 AT 13:20The calculator does a decent job of summarizing known risk factors, but you still need a clinician’s eye to interpret the nuances. Age, gender, and metabolic syndrome each shift the picture in subtle ways. It’s a helpful starting point, not the final word.
Jason Oeltjen
October 18, 2025 AT 05:44While it’s a "helpful start", let’s not ignore the moral responsibility of doctors to double‑check these online tools. Relying blindly is a shortcut that could cost lives.
Mark Vondrasek
October 18, 2025 AT 20:44Oh, look, the risk calculator is ‘fundamentally flawed’. Of course it is-did you ever consider that the data feeding it might be sourced from a corporate lab pushing a hidden agenda? They cherry‑pick TSH thresholds, inflate smoking penalties, and sprinkle metabolic syndrome points like confetti to keep you scared and dependent on pricey follow‑ups. Trusting such a black box without demanding transparency is practically an invitation to be manipulated.
Joshua Agabu
October 19, 2025 AT 13:40I tried the tool with my numbers; it gave me a score of 5, which they label as medium risk. I’m planning to schedule a check‑up just to be safe.
Matthew Bates
October 20, 2025 AT 05:14According to the 2023 ATA guidelines, TSH levels above 10 µIU/mL warrant immediate imaging for vascular complications, which aligns with the calculator’s point allocation for severe hypothyroidism.
NANDKUMAR Kamble
October 20, 2025 AT 19:57There’s a reason they hide the exact weighting of each factor-someone is profiting from the uncertainty.
namrata srivastava
October 21, 2025 AT 12:37The algorithm employs a weighted multivariate regression model, yet the absence of confidence intervals undermines its predictive validity.
Priyanka arya
October 22, 2025 AT 05:00OMG this thing is 🔥! But seriously, if you’re a smoker 🦶 and have metabolic syndrome 🍔, watch out 😬.
Loren Kleinman
October 22, 2025 AT 22:14When we contemplate the interplay between vascular insufficiency and thyroid homeostasis, we uncover a profound reminder that bodily systems are not isolated islands but an intricate tapestry. Each thread-be it hormonal balance, arterial perfusion, or metabolic health-interweaves to shape outcomes that we can only begin to quantify. Tools like this calculator attempt to distill complexity into numbers, offering a map, though never the full territory. Embrace the map, but also listen to the lived experience of your body.
Sabrina Goethals
October 23, 2025 AT 14:20i think it's a good tool, but lol, you gotta double‑check the inputs!!
Amanda Joseph
October 24, 2025 AT 05:20Great, another app to stress me out.
Kevin Aniston
October 24, 2025 AT 22:17Your analogy of the body as a tapestry is spot on. It reminds me that when we tweak one thread-like improving blood flow through exercise-we can reinforce the whole fabric, potentially lowering that risk score you mentioned. Keep sharing these insights; they help us all see the bigger picture.
kiran kumar
October 25, 2025 AT 14:07sure but i think the real issue is they dont even consider diet hormones in the mix its all a scam lol
Brian Johnson
October 26, 2025 AT 04:40True, the guidelines do emphasize imaging at that TSH threshold, but remember that individual variability can affect when you actually need it. Discussing your specific risk with an endocrinologist is still the best path.
Shouvik Mukherjee
October 26, 2025 AT 21:04The lack of confidence intervals is a valid critique; adding them would improve transparency and help clinicians make more informed decisions.
Ben Hooper
October 27, 2025 AT 13:44I’ve been digging into the literature on thyroid‑related ischemia and found a surprisingly consistent pattern across studies.
Patients with elevated TSH often show reduced cerebral perfusion on MRI.
Conversely, low free T4 correlates with endothelial dysfunction in peripheral vessels.
Age over fifty adds a layer of arterial stiffening that amplifies these effects.
Gender differences emerge, with females showing a modestly higher risk, possibly due to hormonal fluctuations.
Smoking introduces oxidative stress that compounds the vascular strain imposed by thyroid imbalance.
Metabolic syndrome contributes insulin resistance, which further impairs microcirculation.
The risk calculator captures these variables in a linear point system, which is a reasonable first approximation.
However, interactions between factors are not purely additive; there are synergistic effects that the model may miss.
For instance, a smoker with metabolic syndrome might experience a greater than expected rise in risk.
Clinical practice guidelines suggest regular vascular assessments for high‑risk thyroid patients.
Ultrasound Doppler and carotid intima‑media thickness measurements are useful tools.
Lifestyle interventions-cessation of smoking, weight management, and controlled iodine intake-can mitigate risk.
Pharmacologically, optimizing levothyroxine dosage to keep TSH within target range reduces vascular strain.
In summary, the calculator is a helpful screening aid, but clinicians should interpret its output within the broader clinical context.