When your child keeps getting ear infections, pneumonia, or thrush that won’t go away, it’s easy to blame it on daycare, bad luck, or a weak immune system. But sometimes, it’s not just bad luck. It could be a sign of something deeper - a primary immunodeficiency. These aren’t rare. About 1 in 1,200 people in the U.S. has one. And if you’re seeing the same infections over and over, especially if they’re serious or don’t respond to antibiotics, it’s time to look beyond the usual explanations.
What Counts as Too Many Infections?
Healthy kids get sick. A lot. Up to 12 respiratory infections a year is normal before age 5. But when infections cross a line - in frequency, severity, or response to treatment - that’s when red flags appear. The American Academy of Allergy, Asthma & Immunology and the European Society for Immunodeficiencies agree on key warning signs:
- Four or more ear infections in one year
- Two or more serious sinus infections in one year
- Two or more pneumonias in one year
- Need for intravenous antibiotics to clear infections
- Two or more deep infections like septicemia or abscesses in organs or skin
- Oral thrush that lasts past age 1
- Infections that don’t improve after two months of standard antibiotics
- Failure to gain weight or grow normally
- Family history of primary immunodeficiency
These aren’t arbitrary numbers. They’re based on decades of data showing that people with conditions like Common Variable Immunodeficiency (CVID) or X-linked agammaglobulinemia consistently hit these thresholds before diagnosis. One study found that kids with CVID had an average of 8 ear infections before age 5 - far beyond the norm. And thrush after age 1? That’s highly specific. One study showed it’s 89% accurate at pointing to antibody deficiency.
It’s Not Always the Immune System
Before jumping to immunodeficiency, doctors need to rule out other causes. About 43% of kids with recurrent infections have anatomical or environmental issues - not immune problems. Cystic fibrosis causes thick mucus that traps bacteria. Chronic sinusitis from deviated septums or polyps creates a perfect breeding ground. Inhaled foreign bodies - like a peanut or toy part - can cause repeated pneumonia in one lung. A 2019 study found 18% of children with recurrent pneumonia had something stuck in their airway.
Even medications can mimic immunodeficiency. Long-term steroids, chemotherapy, or even some autoimmune drugs can lower antibody levels. Up to 30% of adults initially diagnosed with CVID actually had a secondary cause - like lupus, lymphoma, or drug-induced hypogammaglobulinemia. That’s why testing isn’t just about counting infections. It’s about eliminating the look-alikes first.
What the Blood Tests Reveal
Once other causes are ruled out, the workup starts with simple blood tests. The first step is a complete blood count (CBC) with a manual differential. In children over 1, a lymphocyte count below 1,500 cells/μL raises suspicion. In babies under 1, anything under 3,000 is a red flag. Low lymphocytes mean the body’s frontline defenders are missing.
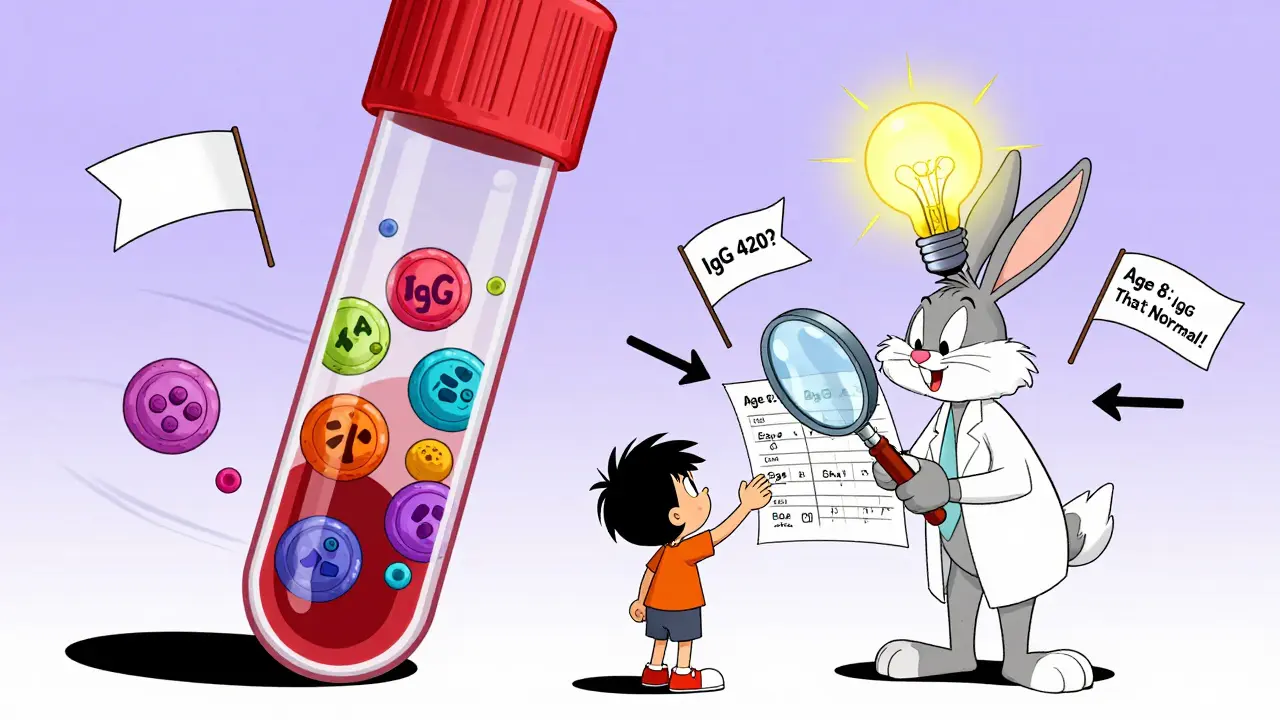
Next, immunoglobulins: IgG, IgA, IgM. But here’s the catch - these numbers change with age. A 3-month-old with an IgG of 243 mg/dL is normal. An 8-year-old with the same level is severely deficient. Many primary care doctors miss this. One pediatrician in Ohio told of three CVID cases missed because their IgG was 420 mg/dL - just above the old cutoff of 400 - but way below what’s normal for their age. The 2022 ARUP Consult reference ranges list 147 different normal values across age groups. You can’t use adult numbers on a child.
Low IgG alone isn’t enough for CVID. You also need low IgA or IgM, and - crucially - poor response to vaccines. That’s where functional testing comes in. After giving a pneumococcal or tetanus vaccine, you wait 4 to 6 weeks and check antibody levels again. Protective levels? At least 0.1 IU/mL for tetanus and 1.3 μg/mL for pneumococcal serotypes. If the body doesn’t make those antibodies, the immune system isn’t working, no matter what the IgG number says.
When to Look Deeper
If basic tests are abnormal or suspicion stays high, flow cytometry is next. This test counts T cells (CD3, CD4, CD8), B cells (CD19), and natural killer cells (CD56). In severe combined immunodeficiency (SCID), T cells are often below 1,000 cells/μL in kids over 2. That’s life-threatening. Without a transplant before 3.5 months, survival drops from 94% to 69%. That’s why newborn screening for SCID is now mandatory in 38 U.S. states - up from just 26 in 2018.
Physical signs matter too. Absent tonsils or lymph nodes? That’s common in SCID - seen in 78% of cases. Skin telangiectasias (tiny red blood vessels) point to ataxia-telangiectasia. Recurrent fungal infections suggest chronic mucocutaneous candidiasis. Growth below the 5th percentile? Seen in 63% of PID cases. These aren’t vague clues. They’re diagnostic anchors.
Genetic Testing Is Changing the Game
For years, diagnosing immunodeficiency meant ruling things out. Now, next-generation sequencing panels can test 484 immune-related genes at once. The StrataID Immune test, approved by the FDA in 2023, finds the genetic cause in 35% of suspected cases - nearly double the rate of older methods. It’s not cheap - around $2,450 - but it cuts years off the diagnostic journey.
Experts predict that within five years, whole exome sequencing will be the first test for suspected immunodeficiencies in developed countries. Right now, the average time from first symptoms to diagnosis is 112 days when following a structured pathway. Without it? Over 400 days. That delay costs lives. One study showed that using the 10-warning-signs checklist reduced diagnostic delay from 9.2 years to just 2.1 years.

What Happens After Diagnosis?
Once you know what’s wrong, treatment can start. For antibody deficiencies like CVID, regular infusions of immunoglobulin (IVIG or SCIG) replace what the body can’t make. For T-cell problems, bone marrow transplants can be curative - if done early. For rare conditions like chronic granulomatous disease, antibiotics and interferon-gamma can prevent infections.
But here’s the catch: you don’t treat based on suspicion. The American College of Physicians found that 22% of patients got immunoglobulin therapy without proof of antibody failure. That’s dangerous. It’s expensive. And it doesn’t fix the root problem. Testing isn’t optional. It’s the only way to know if treatment is needed - and what kind.
Why This Matters Now
More than 485 types of primary immunodeficiencies are now recognized. New ones are still being discovered. And the tools to find them are better than ever. But awareness is still low. In low- and middle-income countries, 78% lack even basic immunoglobulin testing. In the UK and U.S., many doctors still miss the signs because they don’t know the age-adjusted norms.
If you’ve seen a child - or even an adult - with repeated infections that don’t fit the pattern, don’t wait. Don’t assume it’s just a virus. Don’t blame the environment. Ask: Could this be an immune problem? The answer could change everything.





Joe Bartlett
December 16, 2025 AT 23:19My kid had 5 ear infections last year. Doc said it was just daycare. Turns out he had low IgA. We got tested after reading this. Game changer.
Peter Ronai
December 18, 2025 AT 10:08Oh here we go. Another ‘you’re just paranoid’ post from someone who thinks every sniffle is SCID. I’ve seen 12 kids with ‘recurrent infections’ - 11 had asthma or reflux. Stop pathologizing normal childhood. The real epidemic is overtesting.
Steven Lavoie
December 18, 2025 AT 19:52This is one of the clearest, most clinically accurate summaries I’ve read on immunodeficiency red flags. The emphasis on age-adjusted immunoglobulin norms is critical - too many primary care providers still use adult references for pediatric patients. The 2022 ARUP Consult ranges are non-negotiable for accurate interpretation. Thank you for highlighting functional vaccine response testing - that’s the real diagnostic linchpin.
Michael Whitaker
December 19, 2025 AT 16:24Let me be blunt: if you're not ordering flow cytometry after the third pneumonia, you're not doing your job. I've seen too many children languish for years because their pediatrician didn't know CD19 from a hole in the wall. And don't even get me started on the fact that 22% of patients get IVIG without proof of antibody failure - that's malpractice dressed up as precaution.
Anu radha
December 21, 2025 AT 11:59My cousin’s baby had thrush till 2 years old. No one listened. Then one doctor said, ‘Maybe his body can’t fight.’ We tested. It was CVID. Now he gets shots every month. He’s happy now. Thank you for writing this.
Jigar shah
December 22, 2025 AT 07:48Interesting breakdown. I’m curious - how common is it for IgG levels to normalize spontaneously in children under 5 without intervention? I’ve read conflicting reports on whether some kids just ‘grow out of’ low immunoglobulins.
Nishant Desae
December 23, 2025 AT 10:32Man, this hit home. My daughter had 7 ear infections before she turned 3, and I was told ‘she’s just sensitive to cold air.’ Then she got a lung abscess. We were lucky - we found a specialist who knew the 10 warning signs. Took 14 months, but now she’s on SCIG and thriving. I wish I’d known this sooner. To any parent reading this - if your kid’s sick too often and nothing fixes it, push harder. Don’t take ‘it’s normal’ for an answer.
Kaylee Esdale
December 24, 2025 AT 22:36My kid’s got thrush. Again. And I’m done being told it’s ‘just yeast.’ I’m googling ‘CVID symptoms’ and crying in the pediatric waiting room. This post? It’s the first time I felt seen. Thank you.
Jody Patrick
December 26, 2025 AT 17:31US doctors overtest. Europe handles this better. We don’t panic over ear infections. Let kids build immunity. Stop medicalizing childhood.
Raven C
December 27, 2025 AT 09:56How dare you imply that recurrent infections are ever ‘just’ environmental? This is the inevitable consequence of vaccine fatigue, glyphosate exposure, and the collapse of the microbiome due to processed food. The CDC is suppressing the truth - this isn’t immunodeficiency, it’s systemic toxicity. And you’re just part of the pharmaceutical machine profiting off fear.
Donna Packard
December 27, 2025 AT 19:20My son was diagnosed with CVID at 6. We didn’t know what to do. This post? It’s the roadmap we wish we had. You’re helping people. Thank you for the clarity.
Chris Van Horn
December 28, 2025 AT 08:11Let me tell you something - I’ve read every peer-reviewed paper on PID since 2017. You missed the most important point: T-cell dysfunction often precedes antibody failure by years. And you didn’t mention IL-17 pathway defects, which are responsible for 37% of refractory candidiasis cases. Also, your ‘1 in 1,200’ statistic is outdated - the 2024 ESID registry shows 1 in 980. And your ‘$2,450’ quote? That’s the list price. I got StrataID for $890 through my hospital’s research grant. You’re doing a disservice by not citing the real numbers.
Sachin Bhorde
December 29, 2025 AT 09:19As a med student in Mumbai, I’ve seen kids with recurrent pneumonia and zero access to IgG testing. One girl had 4 lung infections in 6 months - we gave her antibiotics till she was 8. Then her cousin got genetic testing in Delhi - turned out to be DOCK8 deficiency. We’re lucky to even have PCR here. This post should be translated to Hindi, Bengali, Tamil - it’s life-saving info. Please share it with global health orgs.
Marie Mee
December 31, 2025 AT 08:46they’re putting tracking chips in the ivig bags. i saw a video. the gov is using immunodeficiency to control the population. your kid gets the shot, they know where you are. why do you think they push this so hard? look at the pharma profits. it’s not about health - it’s about control.
Brooks Beveridge
January 1, 2026 AT 04:17You’re not alone. I’ve been there. The fear. The confusion. The feeling that no one believes you. But you’re doing everything right - asking questions, digging deep, reading the science. That’s how change happens. One test. One diagnosis. One life saved. Keep going. 💪❤️