Lopinavir/Ritonavir Interaction Checker
Check Your Medications
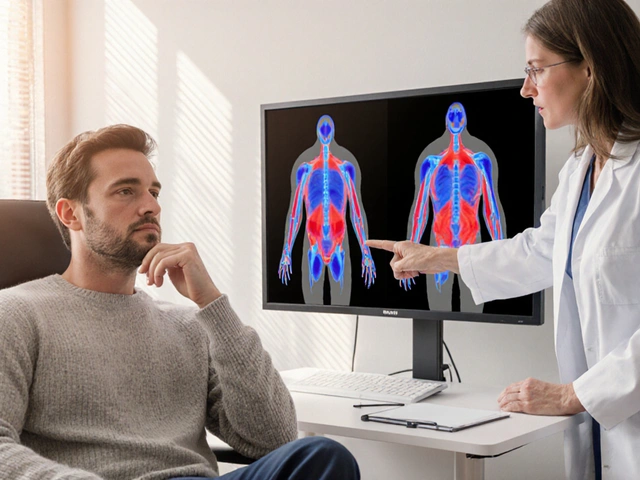
Enter medications you're taking (comma-separated). This tool checks for dangerous interactions with lopinavir/ritonavir based on clinical data from the Liverpool HIV Interactions Database.
Results
Important: This tool is for informational purposes only. Always consult your healthcare provider before making changes to your medications.
When you take lopinavir/ritonavir - commonly known as Kaletra - you’re not just getting two drugs. You’re getting a pharmacological trick designed to make one drug last longer. Ritonavir, at a tiny 100mg dose, doesn’t treat HIV. It exists to shut down a liver enzyme called CYP3A4, which would otherwise break down lopinavir before it can do its job. This trick, called pharmacokinetic boosting, works so well that lopinavir’s half-life jumps from under 7 hours to over 12. But this same trick turns lopinavir/ritonavir into a drug interaction powerhouse - one that can silently mess with dozens of other medications you might be taking.
Why Ritonavir Is the Most Potent CYP3A4 Inhibitor in Clinical Use
Ritonavir doesn’t just block CYP3A4. It destroys it. Unlike most inhibitors that temporarily bind to the enzyme, ritonavir uses four different ways to permanently disable CYP3A4. It latches onto the enzyme’s iron core. It breaks apart its heme group. It sticks reactive fragments to the enzyme’s structure. And it forms a tight, long-lasting complex that won’t let go. The result? CYP3A4 activity drops to less than 15% of normal. That’s why a 100mg dose of ritonavir can boost lopinavir levels by over 500% - even though ritonavir is given at 16 times lower concentration.This isn’t just powerful. It’s unusually complex. Most drugs either inhibit or induce enzymes. Ritonavir does both. It’s a strong inhibitor of CYP3A4 and CYP2D6 - meaning it slows down the breakdown of drugs that rely on those enzymes. But it’s also an inducer of CYP1A2, CYP2B6, CYP2C9, and CYP2C19 - meaning it speeds up the metabolism of other drugs. That dual nature makes predicting interactions harder than with newer boosters like cobicistat, which only inhibits CYP3A4.
The Real-World Cost of Boosting: 1,247 Known Drug Interactions
The Liverpool HIV Interactions Database, updated in July 2023, lists 1,247 drugs that interact with lopinavir/ritonavir. That’s more than 300 interactions higher than the next most problematic boosted regimen. And these aren’t theoretical. They’re documented in real patients.Take warfarin. Ritonavir induces CYP2C9, the enzyme that breaks down warfarin. That means your INR drops - your blood doesn’t clot as slowly as it should. If you’re on warfarin and start lopinavir/ritonavir, you could develop a clot. If you stop the HIV meds, your INR spikes. That’s a dangerous rollercoaster.
Now look at midazolam, a sedative used before surgery. Ritonavir inhibits CYP3A4, which metabolizes midazolam. The result? Midazolam levels can spike by 500%. That’s not just drowsiness - that’s respiratory failure. Anesthesiologists now routinely reduce midazolam doses by 60-80% in patients on ritonavir.
And then there’s rivaroxaban, a blood thinner. It’s contraindicated with lopinavir/ritonavir. The interaction is so dangerous that guidelines say: don’t combine them. Yet patients often don’t know they’re on both. A 72-year-old with atrial fibrillation and HIV might get rivaroxaban from a cardiologist and lopinavir/ritonavir from an infectious disease clinic. Neither doctor may know the other prescribed something.
What Happens When You Combine It With Other Common Drugs?
Here’s what you need to watch for with everyday medications:- Statins (like simvastatin, atorvastatin): Ritonavir increases their levels, raising the risk of muscle damage (rhabdomyolysis). Rosuvastatin is safer, but still needs monitoring.
- Tacrolimus (transplant drug): Levels can double or triple. Dose reductions of 75% are often needed. Without tight blood level checks, kidney failure can follow.
- Methadone: Ritonavir induces its metabolism. Patients report withdrawal symptoms - nausea, sweating, anxiety - even when they haven’t missed a dose. Doses often need to be increased by 20-33%.
- Hormonal contraceptives: Ritonavir cuts estrogen levels by up to 50%. Birth control pills become unreliable. Backup methods aren’t optional - they’re mandatory.
- Voriconazole (antifungal): Ritonavir’s dual action makes levels unpredictable. Sometimes they drop, sometimes they spike. The result? Treatment failure or liver toxicity. It’s contraindicated.
- Fentanyl: Levels can rise 300%. In opioid-naive patients, that’s enough to stop breathing. Even in chronic users, sedation and respiratory depression risk shoots up.
One 2008 study found that when patients on lopinavir/ritonavir were given rifampicin (a TB drug), lopinavir levels dropped by 76%. Hepatotoxicity jumped from 11% to 33%. That’s not a side effect - that’s a clinical disaster.
Why This Matters More Than You Think
Lopinavir/ritonavir isn’t just for HIV anymore. It’s the boosting agent in Paxlovid, the COVID-19 antiviral. That means millions more people are now exposed to ritonavir’s interaction profile - even if they’ve never had HIV.And here’s the twist: the same mechanism that makes Paxlovid work also causes “Paxlovid rebound.” After the 5-day course ends, ritonavir’s inhibition lingers. CYP3A4 is still suppressed. When the body starts making more nirmatrelvir (the active antiviral), it gets cleared too slowly. Levels stay high. Then, when ritonavir finally clears, CYP3A4 rebounds - and nirmatrelvir gets broken down too fast. The virus surges back. It’s not a failure of the drug. It’s a failure of timing - and the complexity of enzyme recovery.
Even in HIV care, lopinavir/ritonavir is fading. In the U.S., it’s used in less than 5% of new HIV starts. Integrase inhibitors like dolutegravir are safer, simpler, and have fewer interactions. But in low-income countries, it’s still a backbone. Why? Cost. In PEPFAR programs, a year of lopinavir/ritonavir costs $68. Dolutegravir? $287. For many, it’s the only option.
What Clinicians Need to Do - And What Patients Should Ask
If you’re prescribing lopinavir/ritonavir, you have to spend 15-20 minutes checking every other drug the patient takes. That’s not optional. The Liverpool database is accessed 2.8 million times a year for a reason. Use it. Don’t guess.For patients: If you’re on this combo, ask these questions:
- “Is anything I’m taking for pain, anxiety, heart issues, or birth control unsafe with this?”
- “Will my blood thinner, cholesterol med, or transplant drug need a dose change?”
- “If I need surgery, what sedatives are safe?”
- “What happens if I start a new antibiotic or antifungal?”
Don’t assume your pharmacist caught it. Don’t assume your doctor remembers. Write down every medication - including OTC painkillers, herbal supplements, and recreational drugs. Bring that list to every appointment.
The Future: Why This Regimen Won’t Disappear - But Should Be Used Less
Lopinavir/ritonavir isn’t going away overnight. It’s still on the WHO Essential Medicines List. It works. It’s cheap. It’s available. But it’s not safe for most people.Research continues into how genetics affect its use. Some people have a variant of CYP3A5 that breaks down lopinavir faster. In those patients, even ritonavir boosting isn’t enough. They need higher doses. But we rarely test for it. That’s a gap in care.
The real lesson? Boosting is powerful - but it’s not magic. It trades simplicity for complexity. It makes one drug work better by making everything else riskier. For most patients today, safer, cleaner alternatives exist. If you’re starting HIV treatment, ask: “Is there a newer option with fewer interactions?” If you’re on lopinavir/ritonavir and taking other meds, ask: “Have we checked every single one?”
Because in the world of drug interactions, the difference between life and death isn’t always the medicine you take. It’s whether you knew what else it was doing to your body.




phenter mine
October 31, 2025 AT 03:25so i just got prescribed this for HIV and didn’t realize how many meds i had to stop… like my statin and that sleep aid i’ve been using for years. my pharmacist caught it but i almost missed it. holy crap this stuff is a minefield.
Aditya Singh
November 2, 2025 AT 02:33Let me correct your misinformed narrative: ritonavir doesn’t merely 'shut down' CYP3A4-it induces irreversible heme destruction via covalent adduct formation, coupled with mechanism-based inactivation that exceeds the inhibitory potency of even clarithromycin or ketoconazole. The 1,247 interactions cited? Underestimated. The Liverpool database includes only FDA-approved agents; when you factor in phytochemicals like St. John’s wort (CYP3A4 inducer) and grapefruit furanocoumarins (irreversible inhibitor), the combinatorial complexity becomes non-linear. Moreover, the claim that cobicistat is 'cleaner' is misleading-it has equally potent inhibition but lacks ritonavir’s CYP2D6 modulation, which paradoxically reduces certain pharmacodynamic conflicts in polypharmacy regimens.
Also, Paxlovid rebound isn’t due to enzyme recovery-it’s a consequence of subtherapeutic nirmatrelvir concentrations post-cessation due to CYP3A4 resynthesis kinetics, which vary by rs2242480 genotype. Most clinicians don’t even screen for CYP3A5*3 expressors, who require 2x higher ritonavir dosing for adequate boosting. This isn’t pharmacology-it’s a clinical minefield disguised as a treatment.
Katherine Reinarz
November 2, 2025 AT 14:16OMG I JUST REALIZED MY MOM IS ON THIS AND ALSO TAKING WARFARIN 😭 I’M CALLING HER RIGHT NOW. I THOUGHT IT WAS JUST FOR HIV BUT SHE’S ON PAXLOVID FOR LONG COVID AND I DIDN’T EVEN THINK ABOUT IT. SHE’S 74 AND I’M SCARED.
John Kane
November 3, 2025 AT 22:36This is one of those posts that makes you realize how much we take for granted in modern medicine. The fact that a 100mg pill can reshape how your entire body processes everything else-painkillers, birth control, even your morning coffee-is both terrifying and awe-inspiring. I’m a nurse in rural Texas, and I see this every day: grandmas on statins, heart meds, and now Paxlovid, all prescribed by different doctors who don’t talk to each other. We need better systems-like automated alerts in EHRs that scream when ritonavir’s in the mix. But until then, patients need to be their own advocates. Write it down. Bring the bag. Ask the hard questions. And if you’re on this combo? Don’t be shy-tell every provider, every time. It might save your life. And hey-if you’re reading this and you’re a clinician? Take 15 minutes. Seriously. The Liverpool database exists for a reason. Use it. It’s not extra work-it’s the work.
Callum Breden
November 4, 2025 AT 05:37This article is dangerously oversimplified. The assertion that 'safer alternatives exist' is a privileged fantasy. In low-resource settings, integrase inhibitors are not merely 'more expensive'-they are inaccessible. To dismiss lopinavir/ritonavir as 'not safe for most people' without acknowledging global equity is not medical insight-it is moral negligence. Furthermore, the claim that CYP3A4 inhibition is 'unusually complex' is trivializing. Every pharmacokinetic booster has nuanced profiles; the difference lies in documentation, not mechanism. The real failure is not the drug-it is the fragmented, siloed, profit-driven healthcare architecture that allows prescribing without coordination. Blame the system. Not the molecule.
Mansi Gupta
November 4, 2025 AT 07:53Thank you for writing this with such clarity. I work in a public health clinic in Delhi, and we still rely heavily on lopinavir/ritonavir due to cost and supply chains. Many patients are unaware of interactions, and we don’t always have access to interaction checkers. We’ve started printing simple handouts with the top 5 risky combinations-warfarin, statins, sedatives, contraceptives, and antifungals-and asking patients to bring all their medications to every visit. It’s not perfect, but it’s something. I hope more clinics adopt this approach. Knowledge should never be a luxury.
Erin Corcoran
November 4, 2025 AT 14:05YESSSS this is why I always make my patients screenshot their med list and send it to me 😅 I had a patient last week on Paxlovid who was also taking melatonin + a turmeric supplement-turns out, turmeric inhibits CYP3A4 too, so we had to delay her surgery by 3 days. She didn’t even think supplements counted! 😳 Always ask about the ‘little stuff’-it’s the little stuff that kills.
shivam mishra
November 6, 2025 AT 03:45As a pharmacist in Mumbai, I’ve seen this play out too many times. A patient comes in for HIV meds, then two weeks later for chest pain and gets a prescription for atorvastatin. No one checks. We caught it because we run automated alerts, but not all pharmacies can. The real tragedy? Patients often stop their HIV meds because they feel ‘too many side effects’-but the side effects aren’t from lopinavir, they’re from the statin toxicity. We need better training for community pharmacists in low-income countries. Not just tech solutions-human ones too. A simple conversation can prevent hospitalization.
Scott Dill
November 6, 2025 AT 09:44Wait-so if ritonavir lingers after Paxlovid, does that mean if I take it again a week later, it won’t work as well? Or is it just the rebound effect? I’ve heard people say they got COVID again after Paxlovid and thought it was the virus fighting back, but now I’m wondering if it’s the drug timing being off. Anyone know if you can re-treat after rebound? I’m just trying to understand if this is a flaw in the drug or a flaw in how we use it.
Arrieta Larsen
November 6, 2025 AT 10:05My dad took this for HIV and ended up in the hospital with rhabdomyolysis because his cardiologist didn’t know he was on Kaletra. He lost 30% of his muscle mass. We almost lost him. I still get sick thinking about it. If you’re on this, don’t wait for your doctor to catch it. Do it yourself. Write it all down. Bring it to every appointment. Seriously. Don’t let it be you.