Fluid Management Calculator for Celiac Disease
Protein Needs Calculator
Sodium Intake Tracker
Daily Management Checklist
- ✅ Read all food labels for hidden gluten
- ✅ Log protein intake daily
- ✅ Keep low-sodium snack options available
- ✅ Measure weight each morning
- ✅ Schedule quarterly blood tests
When Oedema is the accumulation of excess fluid in the body's tissues, often showing up as swelling in the legs, ankles, or even the face meets Celiac Disease an autoimmune reaction to gluten that damages the small intestine and hampers nutrient absorption, the result can be a confusing mix of symptoms.
Quick Takeaways
- Oedema in celiac patients often stems from low protein levels, inflammation, or associated kidney issues.
- Typical signs include swollen ankles, puffy face, and rapid weight gain from fluid retention.
- Diagnosing the link requires blood tests, stool analysis, and sometimes imaging.
- Treatment combines a strict celiac disease gluten‑free diet with fluid‑balance strategies like low‑sodium meals and, when needed, medications.
- Regular follow‑up with a gastroenterologist and a dietitian maximizes recovery.
What Exactly Is Oedema?
In plain language, oedema means “swelling.” It happens when the blood vessels leak fluid into surrounding tissue. The body normally balances fluid through the heart, kidneys, and hormones, but any disruption can tip the scale. Common triggers include heart failure, kidney disease, liver cirrhosis, and certain medications such as diuretics taken in excess.
Key characteristics:
- Visible puffiness, especially in the lower legs and around the eyes.
- Pressing the swollen area leaves a dent (pitting oedema).
- Weight changes that happen overnight.
Understanding Celiac Disease
Celiac disease is a chronic autoimmune disorder. When someone with celiac consumes gluten-found in wheat, barley, and rye-their immune system attacks the lining of the small intestine. This damages tiny finger‑like villi that absorb nutrients, leading to malabsorption.
Typical symptoms include abdominal bloating, diarrhea, anemia, and fatigue. However, many patients present with ‘extra‑intestinal’ signs, like skin rashes, headaches, or, importantly for this article, fluid retention.
How Oedema and Celiac Disease Connect
Even though the two conditions target different systems, they intersect in several ways:
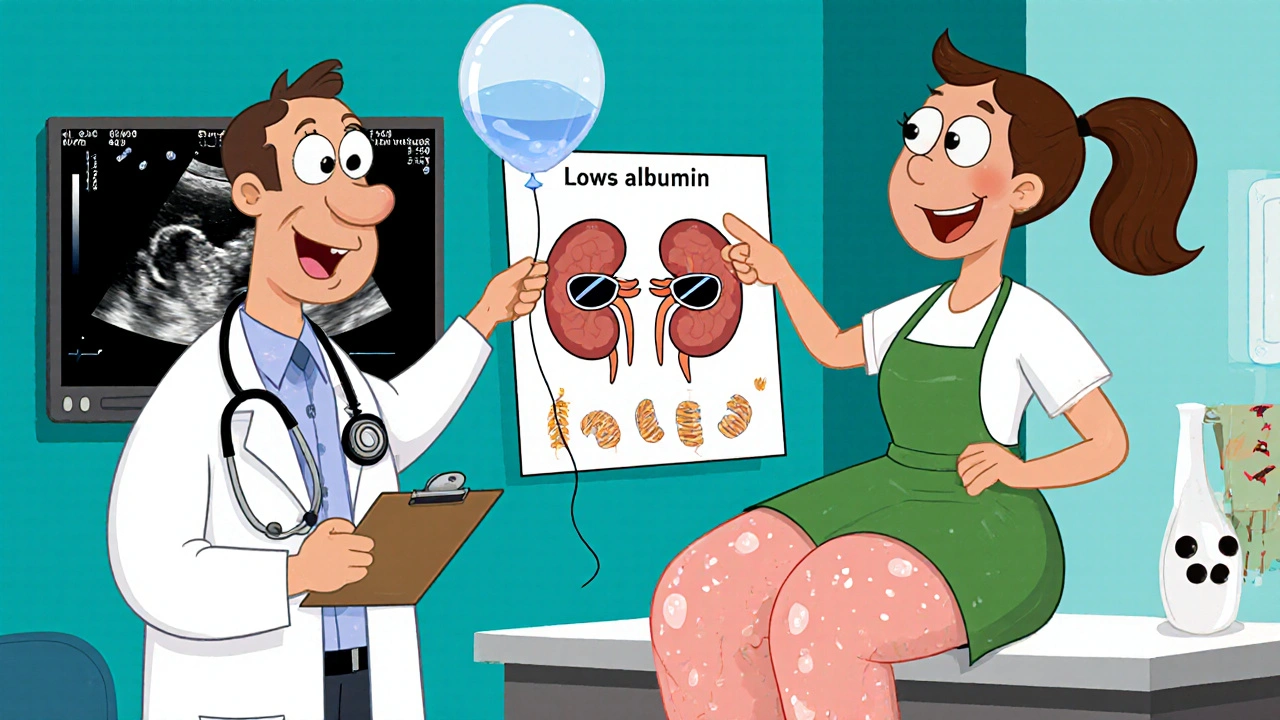
- Protein loss (hypoalbuminemia): Damaged intestinal villi don’t absorb enough protein, lowering blood albumin levels. Albumin helps keep fluid inside blood vessels; low levels push fluid out into tissue.
- Inflammation: Ongoing immune activity releases cytokines that increase vascular permeability, making it easier for fluid to leak.
- Associated kidney issues: Some celiac patients develop IgA nephropathy, a kidney inflammation that impairs fluid removal.
- Medication side effects: Steroids sometimes prescribed for severe celiac complications can cause fluid retention.
Key Causes of Oedema in People With Celiac
Below is a quick rundown of the most common culprits:
- Malabsorption of albumin: Leads to hypoalbuminemia, the classic driver of oedema.
- Chronic inflammation: Cytokine storms increase capillary leak.
- Secondary kidney disease: Reduced filtration amplifies fluid buildup.
- Medication‑induced retention: Steroids, certain antihypertensives, or over‑use of diuretics can backfire.
- Low‑sodium diet reversal: Some patients unintentionally increase salt intake when re‑introducing processed foods after a gluten‑free period.
Recognizing the Symptoms
Because celiac already throws a mix of GI and systemic symptoms at you, oedema can be easy to miss. Keep an eye on these red flags:
- Swollen ankles or calves that don’t improve after sitting or elevating the legs.
- Puffy face, especially around the eyes, noticed first thing in the morning.
- Sudden weight gain of 2‑5 kg within a few days, without changes in diet.
- Feeling tightness in shoes or socks.
- Reduced urine output or darker‑than‑usual urine.
How Doctors Diagnose the Link
Diagnosis is a two‑step dance: confirm celiac, then pinpoint why fluid is building up.
- Blood work: Tissue transglutaminase (tTG) IgA levels for celiac; albumin and creatinine to assess protein status and kidney function.
- Stool analysis: Checks for fat malabsorption, a sign of severe villous damage.
- Imaging: Ultrasound of the abdomen or kidneys to rule out organ‑related causes.
- Biopsy (if needed): Endoscopic sampling of the duodenum confirms celiac damage.
- Medication review: Looking at steroids, antihypertensives, or NSAIDs that could aggravate fluid retention.
Treatment Options - Tackling Both Issues
Successful management rests on treating the root (celiac) and the symptom (oedema). Here’s a practical roadmap.
1. Strict Gluten‑Free Diet
This is non‑negotiable. Eliminating wheat, barley, and rye allows the intestinal lining to heal, restores protein absorption, and reduces inflammation. Consider partnering with a registered dietitian who specializes in celiac to avoid hidden gluten.
2. Boost Protein Intake
While the gut heals, aim for 1.2‑1.5 g of protein per kilogram of body weight daily. Good sources include lean meat, fish, eggs, dairy (if tolerated), and gluten‑free legumes.
3. Manage Sodium
Keep daily sodium under 1500 mg. Opt for fresh fruits, vegetables, and unprocessed meats. Season with herbs, lemon, or vinegar instead of salt.
4. Diuretics - Use With Caution
Short‑term loop diuretics (e.g., furosemide) can relieve severe swelling, but they must be prescribed after kidney function is confirmed. Over‑use can lead to electrolyte imbalances.
5. Treat Underlying Kidney Issues
If IgA nephropathy or another renal problem is present, a nephrologist may suggest ACE inhibitors or ARBs, which both protect kidneys and reduce fluid overload.
6. Supplement Deficiencies
Typical gaps in celiac patients include iron, calcium, vitamin D, and B‑12. Replenish with supplements after blood tests confirm low levels.
7. Lifestyle Tweaks
- Elevate legs above heart level for 15‑20 minutes a few times daily.
- Wear compression stockings if swelling is persistent.
- Stay active - gentle walking improves circulation.
Comparison of Treatment Strategies
| Strategy | Primary Goal | Typical Duration | Key Considerations |
|---|---|---|---|
| Gluten‑free diet | Heal intestinal villi, stop malabsorption | Lifelong | Strict label reading, avoid cross‑contamination |
| Protein enrichment | Raise serum albumin | 4‑12 weeks (until labs improve) | Balance with renal function |
| Low‑sodium diet | Reduce fluid retention | Ongoing | Watch processed‑food hidden salts |
| Diuretics | Quickly lower swelling | Days‑weeks (short‑term) | Monitor electrolytes, kidney health |
| Kidney‑targeted meds (ACE/ARB) | Protect kidneys, lower blood pressure | Months‑years | Check creatinine, potassium |

When to Seek Professional Help
If swelling comes on suddenly, feels painful, or is accompanied by shortness of breath, call your doctor immediately. These can signal heart failure or severe kidney issues, which need urgent care.
Living With Both Conditions
Many people wonder if they’ll be “stuck” with swelling forever. The good news is that once the gut heals and protein levels normalize, oedema often recedes on its own. Consistency is the secret: keep gluten out, stay hydrated (but not over‑hydrated), and monitor your weight weekly.
Quick Checklist for Daily Management
- Read every food label for hidden gluten.
- Log protein intake and aim for the target grams.
- Keep a low‑sodium snack stash (nuts, fresh fruit).
- Measure your weight each morning; flag sudden gains.
- Schedule quarterly blood work to track albumin and kidney markers.
- Schedule a follow‑up with your gastroenterologist every 6‑12 months.
Frequently Asked Questions
Frequently Asked Questions
Can a gluten‑free diet alone fix oedema?
A gluten‑free diet stops the ongoing damage in celiac disease, which often improves protein absorption and reduces inflammation. However, if oedema is already severe, additional steps-like low‑sodium meals, protein supplements, or short‑term diuretics-are usually needed.
Why does my face look puffy in the morning?
Morning puffiness often signals fluid that settled overnight while you slept. In celiac patients, low albumin can let that fluid escape into facial tissues. Elevating your head with an extra pillow and checking your sodium intake can help.
Is it safe to take over‑the‑counter diuretics?
Self‑medicating with OTC diuretics is risky, especially if you have kidney involvement. Always get a prescription and have your doctor monitor electrolytes and kidney function.
What labs should I ask my doctor to check?
Key tests include serum albumin, total protein, creatinine, eGFR, electrolytes (especially potassium), tissue transglutaminase IgA, and a complete blood count for anemia.
Can stress make oedema worse?
Stress releases cortisol, which can cause fluid retention and raise blood pressure. Managing stress with gentle exercise, mindfulness, or adequate sleep can indirectly lessen swelling.



Margaret pope
October 18, 2025 AT 12:32Hey folks, diving deep into the oedema‑celiac link can feel overwhelming but you’re not alone. First, understand that low albumin is the core driver of fluid leaking into tissues. When the gut can’t absorb protein the blood loses its oncotic pressure and swelling follows. This cascade starts with villous atrophy that you see in celiac disease. The damaged villi reduce amino acid uptake and low serum albumin follows. With less albumin, water shifts out of the vasculature into interstitial spaces. That’s why you notice puffy ankles and a bloated face in the mornings. In addition, chronic inflammation ramps up cytokine production which makes capillaries leaky. The immune system’s constant alert in celiac also taxes the kidneys over time. Some patients even develop IgA nephropathy which impairs fluid clearance. All of these mechanisms converge to produce oedema. Managing it starts with a strict gluten‑free diet to let the gut heal. As the intestinal lining repairs, protein absorption improves and albumin levels rise. Pair that with a targeted increase in high‑quality protein sources such as lean meat, eggs, and legumes. Keep sodium intake below 1500 milligrams per day to prevent excess fluid retention. Simple lifestyle tweaks like leg elevation, compression stockings, and gentle walking boost circulation. If swelling is severe, short‑term diuretics can be prescribed, but always under medical supervision. Regular blood work tracking albumin, creatinine, and electrolytes guides therapy. Remember, consistency is key and you’ll likely see the puffiness recede as your gut recovers. Stay patient, stay supported, and keep the dialogue open with your healthcare team.
Liberty Moneybomb
October 19, 2025 AT 10:45Look, the powers that be don’t want you to connect the dots – they thrive on your swelling and confusion. They sprinkle hidden gluten into “gluten‑free” snacks while whispering that a little salt won’t hurt, all to keep you hooked on their processed food empire. It isn’t a coincidence that the pharma industry pushes diuretics as a quick fix, masking the real culprit: a compromised gut silently sabotaging your body. Every time you feel that puffiness in the morning, think of the hidden agenda pulling the strings behind your plate. The medical establishment loves to downplay the nutrient loss, but the truth is staring you right in the face – low protein levels are the silent weapon they ignore. Don’t be a pawn; demand full transparency on lab results and scrutinize every label as if your life depends on it – because it does.
Alex Lineses
October 20, 2025 AT 08:58Let’s break this down with the proper terminology so you can see the full picture. In celiac disease, the autoimmune assault triggers villous atrophy, leading to malabsorption of essential macronutrients, particularly albumin, which is a key plasma oncotic agent. Hypoalbuminemia, in turn, precipitates a decrease in oncotic pressure, allowing extravascular fluid shift – the hallmark of pitting oedema. Moreover, pro‑inflammatory cytokines such as IL‑6 and TNF‑α increase vascular permeability, compounding the fluid extravasation. If renal involvement like IgA nephropathy is present, glomerular filtration rate declines, further impairing fluid homeostasis. Your therapeutic plan should therefore be three‑pronged: a strict gluten‑free diet to restore intestinal integrity, targeted protein supplementation to rebuild serum albumin, and a low‑sodium regimen to curb sodium‑induced water retention. Pair these with regular monitoring of serum albumin, eGFR, and electrolyte panels to gauge progress. Stay disciplined, and you’ll see the oedema subside as your gut heals and your labs normalize.
Brian Van Horne
October 21, 2025 AT 07:12Elevate those legs and the swelling will ease.
Norman Adams
October 22, 2025 AT 05:25Oh, because obviously a gluten‑free diet is just a whimsical lifestyle trend and not a medically mandated intervention, right? It’s amusing how the “simple” solution of avoiding wheat is dismissed as a fad while the real science is buried under a mountain of culinary mythology. One would think that restoring protein absorption and correcting hypoalbuminemia would be obvious, yet the discourse drifts into endless anecdote. Perhaps we should all convene a symposium on the profound complexities of “just eat less salt” while ignoring the autoimmune foundation.
Rajesh Singh
October 23, 2025 AT 03:38Let us not be seduced by the allure of intellectual posturing when real lives hang in the balance. The moral imperative is clear: patients deserve earnest guidance, not a circus of sarcasm that trivializes their suffering. When we reduce a serious malabsorption syndrome to a “trend,” we betray the very principles of compassionate care. It is our duty to champion evidence‑based treatment, to lift the veil of ignorance, and to advocate for those whose bodies are waging silent wars. Anything less is an affront to both science and humanity.
Albert Fernàndez Chacón
October 24, 2025 AT 01:52I get how frustrating it can be to juggle the diet changes and the swelling at the same time. A good start is to keep a simple food diary and note any salty snacks that sneak in – those can sneakily add up. Make sure you’re hitting that protein goal each day; a handful of nuts or a boiled egg can make a difference. If the legs feel heavy, try propping them up for a few minutes after you sit or stand for a while. And don’t forget to check in with your dietitian regularly – they can spot hidden gluten and keep you on track.
Drew Waggoner
October 25, 2025 AT 00:05Every time I hear “just keep a diary,” I feel the weight of endless monitoring crushing my spirit. The relentless cycle of counting protein grams, fearing hidden gluten, and watching the puffiness grow is a torment that never truly ends. It’s as if the body conspires to remind you of its fragility with every swollen ankle, draining any spark of optimism. The only respite seems to be the fleeting hope of a lab result that finally says “you’re improving,” yet even that is a fleeting lighthouse in a storm of perpetual vigilance.