Potassium Intake Calculator for ACE Inhibitor Users
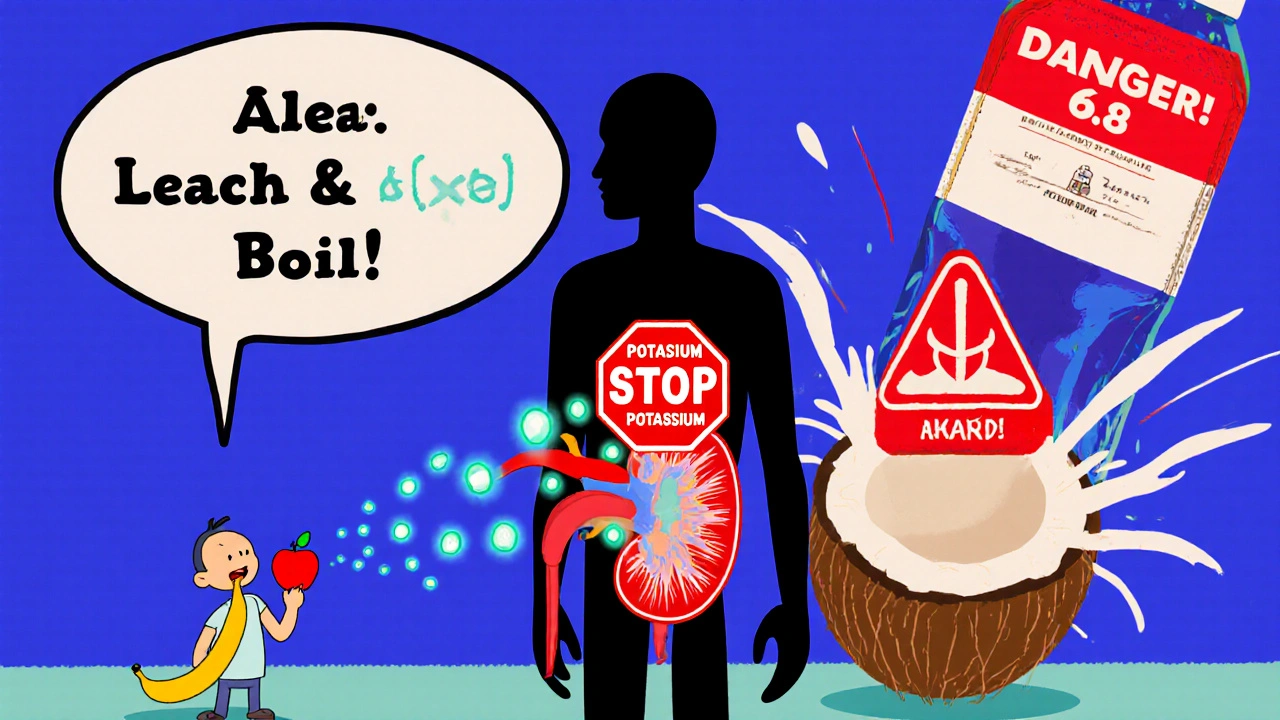
When you're taking an ACE inhibitor for high blood pressure, heart failure, or kidney disease, you're getting real protection for your heart and kidneys. But there’s a quiet danger hiding in plain sight: your food. Some of the healthiest foods you eat-bananas, potatoes, spinach, avocados-can push your potassium levels too high, especially when your body can't flush it out properly. That’s when hyperkalemia happens. And it’s not just a lab number you ignore. High potassium can cause irregular heartbeats, muscle weakness, and even cardiac arrest. The good news? You can manage it. You don’t have to give up healthy eating. You just need to know what to watch for.
Why ACE Inhibitors Raise Potassium Levels
ACE inhibitors like lisinopril, enalapril, and ramipril work by blocking a hormone system called RAAS. This system normally tells your kidneys to get rid of extra potassium. When ACE inhibitors shut it down, your body holds onto more potassium than it should. It’s not the drug itself that’s toxic-it’s what it stops your body from doing. Within 24 hours of taking your first dose, your kidneys start holding onto potassium instead of flushing it out. For healthy people, that’s not a big deal. But if you have kidney problems, diabetes, or are over 75, your body doesn’t handle the change well.Studies show that between 10% and 24% of people on ACE inhibitors develop high potassium levels. That number jumps to over 40% if you already have chronic kidney disease (eGFR under 60). Diabetic patients are at even higher risk-47% more likely to develop hyperkalemia than non-diabetics on the same meds. And if you’re also taking a potassium-sparing diuretic like spironolactone, or even certain antibiotics like trimethoprim, your risk doubles or triples.
Which Foods Are the Biggest Risks
You don’t need to avoid all fruits and vegetables. But you do need to know which ones pack the most potassium-and how much you can safely eat. The National Kidney Foundation recommends keeping daily potassium under 2,000 mg if your kidney function is below 45 mL/min. Here’s what that looks like in real portions:- One medium banana = 422 mg
- One baked potato = 926 mg
- One cup cooked spinach = 839 mg
- One medium tomato = 292 mg
- One avocado = 708 mg
- One cup orange juice = 496 mg
- One cup cooked lentils = 731 mg
- 16 oz coconut water = 1,150 mg
It’s not just the obvious suspects. Many people don’t realize that protein powders, salt substitutes (which often contain potassium chloride), and even some low-sodium canned soups are loaded with potassium. One Reddit user shared that after drinking a large bottle of coconut water-thinking it was a healthy hydration boost-he ended up in the ER with a potassium level of 6.8. That’s life-threatening.
Who’s Most at Risk
Not everyone on ACE inhibitors needs to follow strict potassium limits. Risk depends on three things: kidney function, age, and other health conditions.- Chronic kidney disease (CKD) stages 3-5: Your kidneys can’t excrete potassium well. The higher your stage, the stricter your limits need to be.
- Diabetes: Even mild kidney damage from diabetes raises your risk. If you have protein in your urine (albuminuria), your chances of hyperkalemia jump.
- Age 75+: Kidney function naturally declines with age. Older adults need closer monitoring.
- Heart failure (NYHA Class III-IV): These patients often take multiple drugs that affect potassium, making them more vulnerable.
- On other potassium-raising meds: Spironolactone, eplerenone, trimethoprim, NSAIDs, and some herbal supplements can stack up the risk.
If you fall into any of these groups, your doctor should check your potassium and kidney function before starting an ACE inhibitor-and again 7 to 14 days after starting or changing your dose. After that, every 4 months is standard. If your creatinine rises by more than 30% or your potassium goes above 5.0 mmol/L, your dose may need to be lowered or your diet adjusted.

How to Eat Smart Without Giving Up Nutrition
You don’t have to become a food scientist. But you do need to make a few smart swaps.Leach your vegetables. Potassium in potatoes, carrots, and beets can be reduced by peeling, cutting into small pieces, and soaking in warm water for 2+ hours before cooking. Then boil them in plenty of water and discard the water. This can cut potassium by up to 50%.
Choose lower-potassium fruits. Apples, berries, grapes, pineapple, and watermelon are safer options. Swap orange juice for apple juice. Pick canned peaches in juice (not syrup) over fresh.
Watch portion sizes. One banana a day might be too much. Two small servings of spinach in a salad? Fine. A whole pot of cooked spinach? Not if your kidneys are weak.
Avoid salt substitutes. These often contain potassium chloride instead of sodium chloride. They’re marketed as healthy, but for you, they’re dangerous.
Read labels. Look for potassium chloride, potassium lactate, or potassium phosphate on ingredient lists. They’re hidden in many processed foods, especially low-sodium or “heart-healthy” products.
What Works Better Than Guessing
Many patients struggle to keep track of potassium. A 2022 study found that 68% couldn’t name three high-potassium foods. That’s why simple tools help:- Laminated food charts from your pharmacy or clinic show potassium content at a glance.
- Apps like Renal Diet Helper let you scan barcodes or search foods and track daily intake.
- Meeting with a renal dietitian cuts your risk of hyperkalemia by 34%. One program (KEEP) found that patients who got both written materials and in-person coaching had 42% better adherence than those who just got handouts.
Don’t wait until you feel sick. Hyperkalemia often has no symptoms until it’s too late. Fatigue, muscle cramps, or an irregular heartbeat might be your only warning. That’s why regular blood tests are non-negotiable.
New Tools to Help You Stay on Your Meds
For years, doctors had to choose between protecting your heart and avoiding high potassium. Now, there’s a third option: potassium binders.Drugs like patiromer (Veltassa) and sodium zirconium cyclosilicate (Lokelma) work in your gut to trap potassium before it enters your bloodstream. Clinical trials show they reduce the need to stop ACE inhibitors by 41%. That means you can keep taking the meds that save your life-without the danger.
These aren’t magic pills. You still need to watch your diet. But they give you breathing room. If your potassium keeps creeping up despite diet changes, ask your doctor if one of these binders might help.
What’s Next for Treatment
Researchers are working on new drugs that block the RAAS system without messing up potassium. One compound, KBP-5074, is in phase 2 trials. In early results, 82% of patients with CKD kept their potassium in the normal range-compared to just 54% on placebo. If this works, it could change how we treat high blood pressure in kidney patients forever.But for now, the best defense is still simple: know your numbers, know your food, and talk to your care team. Don’t stop your ACE inhibitor because you’re scared of potassium. But don’t ignore it either. With the right plan, you can eat well, stay healthy, and keep your heart protected.
Can I still eat bananas if I’m on an ACE inhibitor?
You can, but you need to be careful. One medium banana has about 422 mg of potassium. If your kidney function is normal and your potassium levels are stable, one banana a day is usually fine. But if you have chronic kidney disease, diabetes, or your potassium has been high before, you should limit bananas to once or twice a week-or swap them for lower-potassium fruits like apples or berries. Always check your blood levels before making big changes.
Is it safe to use salt substitutes on ACE inhibitors?
No. Most salt substitutes replace sodium chloride with potassium chloride. One teaspoon can contain over 1,000 mg of potassium-more than half your daily limit if you have kidney disease. Even if you think you’re being healthy, this can spike your potassium dangerously. Stick with regular salt in small amounts, or use herbs and spices instead.
How often should I get my potassium checked on ACE inhibitors?
Before starting the medication, get a baseline blood test. Then, check again 7 to 14 days after starting or changing your dose. After that, every 4 months is standard for most people. If you have kidney disease, diabetes, or are over 75, your doctor may want to check every 2 to 3 months. Never skip these tests-even if you feel fine.
Can drinking too much water lower my potassium?
No. Drinking extra water won’t help your kidneys flush out potassium if they’re already struggling. In fact, overhydration can dilute your sodium and cause other problems. The key isn’t how much you drink-it’s whether your kidneys can excrete potassium. If your eGFR is low, your body can’t use water to fix high potassium. Focus on diet and medication management instead.
What should I do if my potassium is high but I can’t stop my ACE inhibitor?
Talk to your doctor about potassium binders like patiromer (Veltassa) or sodium zirconium cyclosilicate (Lokelma). These medications trap potassium in your gut so it doesn’t enter your blood. They’re not a replacement for diet changes, but they let you keep taking your life-saving ACE inhibitor without risking dangerous spikes. Many patients find this combination works better than stopping the drug entirely.




Amy Hutchinson
November 25, 2025 AT 03:59I just ate a banana with my oatmeal this morning and now I’m sweating and my arm feels numb. I swear, if I die because of this, someone’s gonna get sued. ACE inhibitors are basically slow poison with a prescription label. I’m not even kidding. My cousin’s neighbor’s dog had a heart attack after eating a potato peel. It’s all connected.
Archana Jha
November 26, 2025 AT 02:59ok so here’s the thing no one talks about but the real cause of hyperkalemia is not the food or the drug its the government’s secret potassium control program in the water supply they add it to make us docile and stop us from questioning the system also i heard the FDA is in cahoots with big banana and big avocado to keep us scared of our own kitchens lol
Aki Jones
November 27, 2025 AT 16:24Let’s be clear: this isn’t about diet. It’s about systemic pharmaceutical negligence. The RAAS axis suppression isn’t a side effect-it’s a feature. The FDA approved these drugs knowing the potassium cascade would force patients into more expensive, profit-driven interventions-binders, labs, specialist visits. And don’t even get me started on the coconut water industry. They’re not selling hydration. They’re selling cardiac arrest disguised as wellness. I’ve read the clinical trial metadata. It’s all rigged.
Jefriady Dahri
November 28, 2025 AT 02:38Hey everyone, I’m a nurse in Kerala and I’ve seen so many patients struggle with this. Don’t panic-just be smart! 🙌 You can still enjoy your veggies-just leach ‘em, watch portions, and get your labs done. I had a 78-year-old grandma who swapped her banana for apple slices and now she’s hiking every morning. You got this! 💪
Sharley Agarwal
November 28, 2025 AT 15:26People are dying because they think they’re healthy. You’re not. You’re just lucky.
Shivam Goel
November 30, 2025 AT 03:15Let’s quantify this: 422 mg per banana? That’s 21.1% of your daily limit if you’re CKD stage 4. But here’s the real math-your eGFR of 38 means your kidneys excrete 0.8 mL/sec of potassium. One banana = 1.2 seconds of excretion capacity consumed. You’re not eating a banana. You’re doing a 1.2-second cardiac stress test. And if you’re on spironolactone? You’re not eating-you’re self-administering a lethal cocktail. The fact that this isn’t a black box warning is criminal.
Andrew Camacho
December 2, 2025 AT 01:51Oh wow, so now we’re blaming bananas? Next they’ll say the sun is causing heart attacks. This is why people hate doctors-because you make healthy things sound like weapons. I’ve been on lisinopril for 8 years, eat 3 bananas a day, and my potassium is 4.1. Your fear-mongering is more dangerous than the drug. You’re creating anxiety disorders in people who just want to live. Grow up.
Arup Kuri
December 3, 2025 AT 06:51My uncle died from this. He was told to eat healthy so he ate spinach every day. He didn't know potassium was poison. The doctors didn't tell him. The system failed him. Now I don't trust anything on a label. Not even water. You think you're safe? You're not.
Elise Lakey
December 4, 2025 AT 18:16Thanks for this. I’m on lisinopril and just got my first blood test back-potassium was 5.2. I didn’t realize coconut water was that bad. I’ve been drinking it daily because I thought it was ‘natural.’ I’m switching to apple juice and will ask my doctor about binders. This post literally saved me.