Key Takeaways
- DRESS syndrome is a life‑threatening drug reaction that usually appears 2-8 weeks after exposure to a high‑risk medication.
- The RegiSCAR scoring system is the gold‑standard for diagnosis, offering >90% sensitivity when viral reactivation markers are included.
- Immediate drug withdrawal, systemic corticosteroids, and close organ monitoring are the cornerstone of treatment.
- HLA‑B*58:01 and HLA‑A*31:01 screening dramatically lowers incidence for allopurinol and carbamazepine.
- Long‑term follow‑up is essential because up to 30% of survivors develop chronic autoimmune sequelae.
DRESS syndrome is a severe cutaneous adverse reaction (SCAR) that combines a widespread rash, fever, eosinophilia, and multi‑organ involvement after a drug trigger. It is also known as drug‑induced hypersensitivity syndrome (DIHS) and carries a mortality rate of about 10%. Early recognition saves lives, but the latency period of 2-8 weeks often blinds clinicians who expect reactions to happen within days.
DRESS syndrome demands a systematic approach: stop the offending drug, confirm the diagnosis with RegiSCAR, assess organ damage, and start systemic therapy without delay.
What Is DRESS and Why Does It Matter?
The syndrome was first described in 1950 as phenytoin hypersensitivity and formally named DRESS in 1996. It sits between acute generalized exanthematous pustulosis (AGEP) and Stevens‑Johnson syndrome/toxic epidermal necrolysis (SJS/TEN) in severity. Unlike SJS/TEN, DRESS features prolonged fever, facial edema, and striking eosinophilia (>1,500 cells/µL). The systemic inflammation can cripple the liver, kidneys, lungs, heart, or pancreas, making it a true medical emergency.
Epidemiology & Risk Factors
Incidence varies from 1 per 1,000 to 1 per 10,000 drug exposures, with higher rates in Asia (up to 15 per 10,000 hospital admissions). High‑risk drugs account for most cases:
- Allopurinol - ~28% of reports
- Carbamazepine - ~24%
- Various antibiotics (especially vancomycin) - ~20%
- Anticonvulsants (lamotrigine, phenytoin) - ~15%
Genetic predisposition is key. HLA‑B*58:01 carriers have an 80% higher odds of allopurinol‑related DRESS, while HLA‑A*31:01 raises carbamazepine risk. Nations that mandate pre‑prescription HLA screening (e.g., Taiwan) have cut incidence by up to 80%.
Clinical Presentation
Typical signs appear 2-8 weeks after drug start:
- Rash: morbilliform, often beginning on the face and upper trunk, spreading to cover 80‑90% of body surface within days.
- Facial edema (≈68% of cases) and lip crusting (≈52%).
- Fever >38.5 °C in 98% of patients.
- Lymphadenopathy (≈75%).
- Eosinophilia >1,500 cells/µL in 70% and atypical lymphocytes in 60%.
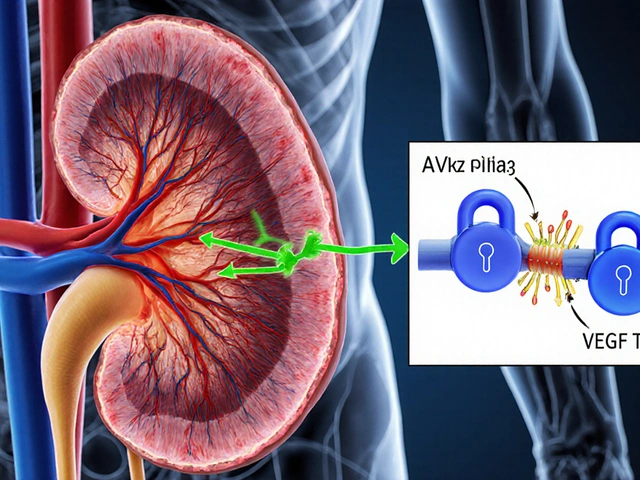
Organ involvement is the rule, not the exception (≈90% of cases). The liver is hit most often - ALT can exceed 300 IU/L, sometimes soaring past 1,000 IU/L. Renal, pulmonary, cardiac, and pancreatic injury occur less frequently but dramatically increase mortality.
How DRESS Differs From Other SCARs
| Feature | DRESS | SJS/TEN | AGEP |
|---|---|---|---|
| Latency (after drug) | 2-8 weeks | 4-28 days | 1-2 days |
| Typical skin pattern | Morbilliform, facial edema | Target lesions, extensive epidermal detachment | Acute sterile pustules |
| Eosinophilia | Yes, >1,500 cells/µL | Rare | Occasional |
| Organ involvement | 90% (liver most common) | 30-40% (skin‑dominant) | Minimal |
| Mortality | ~10% | 25-35% | <5% |
| Key diagnostic tool | RegiSCAR score | Clinical + skin biopsy | Clinical + pustule culture |
These differences help clinicians avoid misdiagnosis - a common problem that delays proper care by an average of 19 days.
Diagnosing DRESS: The RegiSCAR Scoring System
Developed in 2007 and updated in 2023, RegiSCAR assigns points for seven criteria: fever, enlarged lymph nodes, eosinophilia, atypical lymphocytes, skin rash extent, organ involvement, and exclusion of alternative diagnoses. A score ≥5 is "definite" DRESS, 4 is "probable," and ≤3 is "possible." Adding viral reactivation markers (HHV‑6, EBV, CMV) boosts sensitivity from 80% to 92%.
Practical steps:
- Discontinue every non‑essential medication immediately (within 24 h of suspicion).
- Order CBC with differential, LFTs, serum creatinine, and urinalysis.
- Screen for HHV‑6 DNA, EBV IgM, CMV PCR, and hepatitis serologies.
- Calculate RegiSCAR points. Use the freely available mobile app for quick scoring.
- Document HLA genotype if the culprit drug is known (e.g., HLA‑B*58:01 for allopurinol).
Management Principles
There is no randomized trial that definitively proves a single regimen, but observational data converge on three pillars:
- Drug withdrawal - the most decisive factor; delays beyond 48 h raise mortality by 2‑fold.
- Systemic corticosteroids - oral prednisone 1 mg/kg/day or IV methylprednisolone for severe organ damage. Taper over 3-6 months, reducing 5-10 mg weekly once labs normalize.
- Organ‑specific support - ICU monitoring for ALT >1,000 IU/L, creatinine >2.0 mg/dL, or respiratory failure; consider N‑acetylcysteine for liver injury, renal replacement therapy if needed.
Adjuncts gaining traction:
- IVIG (2 g/kg over 2‑3 days) - helpful when viral reactivation is documented.
- Mycophenolate mofetil - steroid‑sparing alternative in chronic cases.
- Cyclosporine - used in some Asian cohorts with rapid eosinophil decline.
Always involve a multidisciplinary team: dermatology, internal medicine, infectious disease, and pharmacy.
Prognosis, Follow‑Up, and Long‑Term Risks
Survivors face a 30% chance of developing autoimmune thyroiditis, type 1 diabetes, or lupus‑like syndromes within two years. Regular follow‑up labs every 3 months for the first year are recommended. Patients should also be educated about future drug avoidance and the need for HLA testing before re‑exposure to high‑risk agents.

Current Research & Emerging Tools
Key developments in 2023‑2025 include:
- The FDA‑cleared point‑of‑care HLA‑B*58:01 test (Verigene) enables same‑day screening before allopurinol prescription.
- Phase 2 trials combining IVIG with mycophenolate show 70% remission at 12 weeks, offering a steroid‑sparing pathway.
- A global DRESS registry now hosts >1,200 cases, providing real‑world data on drug culprits and outcomes.
- Biomarker panels incorporating cytokine spikes (IL‑5, IL‑13) aim to predict chronic autoimmune sequelae.
Within the next five years, experts predict universal HLA screening for all high‑risk drugs, potentially slashing incidence by 60‑70%.
Practical Checklist for Clinicians
- Suspect DRESS if fever + rash + eosinophilia appear 2-8 weeks after a new medication.
- Stop the drug immediately; document the action.
- Order labs: CBC, LFTs, renal panel, viral PCRs, and HLA typing if relevant.
- Calculate RegiSCAR score; aim for ≥5 before confirming.
- Start systemic steroids; plan a slow taper.
- Monitor organ function daily for the first 72 hours, then every 48 hours until stable.
- Consider IVIG or steroid‑sparing agents for refractory or steroid‑intolerant patients.
- Arrange multidisciplinary case review and discharge planning with dermatology follow‑up.
Patient Stories: The Human Side of DRESS
On the DRESS Syndrome Foundation forum, 78% of respondents described multiple ER visits before a correct diagnosis. One patient, a 34‑year‑old teacher on lamotrigine, spent three weeks in the hospital before her liver enzymes spiked to 1,200 IU/L, prompting a DRESS diagnosis and a 10‑week prednisone taper. She now advocates for HLA screening in primary care.
Conversely, a 42‑year‑old man with carbamazepine‑induced DRESS suffered permanent renal damage because his kidney function deteriorated unnoticed for 22 days. This case underscores why early organ monitoring is non‑negotiable.
Bottom Line
DRESS syndrome sits at the intersection of dermatology, immunology, and internal medicine. Prompt drug cessation, rigorous use of the RegiSCAR tool, and early systemic therapy are the only proven ways to tilt the odds toward survival and recovery. As genetics and rapid diagnostics improve, the future looks brighter, but clinicians must stay vigilant today.
What drugs are most commonly linked to DRESS?
Allopurinol, carbamazepine, various antibiotics (especially vancomycin), and anticonvulsants such as lamotrigine and phenytoin together account for roughly 80% of reported cases.
How long after starting a medication can DRESS appear?
The typical latency is 2-8 weeks, though rare cases have been documented up to 12 weeks after exposure.
What is the RegiSCAR score and how is it used?
RegiSCAR assigns points for fever, lymphadenopathy, eosinophilia, atypical lymphocytes, rash extent, organ involvement, and exclusion of other causes. A total of 5 or more points indicates a definite case of DRESS.
Why is HLA screening important?
Specific HLA alleles (e.g., HLA‑B*58:01 for allopurinol, HLA‑A*31:01 for carbamazepine) dramatically increase DRESS risk. Pre‑prescription testing can prevent up to 80% of cases in populations where the allele is common.
Can corticosteroids be stopped abruptly?
No. A gradual taper over 3-6 months reduces relapse risk and helps the immune system rebound safely. Abrupt cessation can trigger rebound inflammation and organ damage.
What long‑term complications should patients expect?
Up to 30% develop autoimmune disorders such as thyroiditis, type 1 diabetes, or systemic lupus erythematosus. Regular labs and clinical review are advised for at least two years after recovery.




Nic Floyd
October 26, 2025 AT 11:27When you’re juggling allopurinol and carbamazepine the immune system can go into overdrive 🚀 the RegiSCAR algorithm gives you a quantitative readout and cuts diagnostic ambiguity down to almost zero the eosinophil count above 1,500 cells/µL is the red flag and you should pull the culprit drug pronto the cytokine surge, especially IL‑5, explains why steroids work so fast 🤒
Johnae Council
November 4, 2025 AT 17:41Nice rundown but the guide glosses over the fact that many hospitals still lack rapid HLA testing, leaving clinicians stuck with guesswork.
Manoj Kumar
November 13, 2025 AT 23:54Ah, the classic 2‑8 week cliff‑hanger, as if drugs enjoy dramatic timing. In reality your immune system is staging a philosophical debate with the drug’s metabolite-spoiler: the immune side usually wins. So keep your eyes peeled, not just your labs.
Rhea Lesandra
November 23, 2025 AT 06:07Colleagues, let’s take a moment to appreciate how DRESS forces us to practice truly interdisciplinary medicine. First, the skin presentation is just the tip of the iceberg, and recognizing it early can prevent organ damage. Second, remember that any new medication started within the past three months is a potential trigger, even if it’s a vitamin supplement. Third, the RegiSCAR score is not a bureaucratic hurdle; it’s a lifesaver that quantifies fever, lymphadenopathy, eosinophilia, atypical lymphocytes, rash extent, and organ involvement in a single number. Fourth, do not underestimate the value of baseline labs before initiating high‑risk drugs; they give you a reference point for detecting rapid ALT spikes. Fifth, HLA‑B*58:01 and HLA‑A*31:01 testing should become standard of care in any clinic that prescribes allopurinol or carbamazepine, because the cost of a rapid test is dwarfed by the expense of a prolonged ICU stay. Sixth, systemic corticosteroids remain the cornerstone of therapy, but taper them slowly over three to six months to avoid rebound inflammation. Seventh, if steroids are contraindicated or the patient shows steroid‑refractory disease, consider adjuncts such as IVIG, cyclosporine, or mycophenolate, each backed by emerging evidence. Eighth, organ monitoring should be daily for the first 72 hours and then every 48 hours until trends stabilize; liver enzymes, creatinine, pulmonary function, and cardiac enzymes are all part of the checklist. Ninth, involve dermatology early, because a skin biopsy can help differentiate DRESS from AGEP or acute SJS/TEN. Tenth, educate patients at discharge about drug avoidance and the importance of carrying an HLA test result card; many future reactions can be prevented with a simple alert. Eleventh, schedule follow‑up visits at three‑month intervals for at least two years because autoimmune sequelae such as thyroiditis or type‑1 diabetes can emerge long after the rash fades. Twelfth, contribute data to the global DRESS registry; collective experience accelerates the refinement of diagnostic criteria. Thirteenth, keep an eye on viral reactivation markers like HHV‑6, as they can guide the use of antiviral therapy. Fourteenth, remember that empathy matters: patients often feel abandoned after multiple ER visits before a diagnosis, so clear communication can improve adherence to therapy. Finally, stay curious, stay collaborative, and never assume the reaction will resolve without vigilant follow‑up.
Kasey Marshall
December 2, 2025 AT 12:21Great summary I’ll add that checking renal function early can catch hidden injury before it escalates
Erin Leach
December 11, 2025 AT 18:34I appreciate how the guide balances detail with practical steps, it makes it easier for busy clinicians to act quickly.
Erik Redli
December 21, 2025 AT 00:47Honestly the obsession with HLA screening is overblown; most patients never develop DRESS and the costs outweigh the benefits.
Tim Waghorn
December 30, 2025 AT 07:01While cost considerations are valid, numerous studies demonstrate a reduction in allopurinol‑induced DRESS incidence by up to 80 % when HLA‑B*58:01 screening is implemented, justifying the expense in high‑risk populations.
Jay Campbell
January 8, 2026 AT 13:14Early drug withdrawal saves lives.
Laura Hibbard
January 17, 2026 AT 19:27Wow, groundbreaking insight, I’m sure no one has ever said that before.
Rachel Zack
January 27, 2026 AT 01:41It’s a responsibility of the medical community to not ignore the severe side effects of these drugs, they must be held accountable for preventable harm.
Lori Brown
February 5, 2026 AT 07:54Let’s keep pushing for universal HLA testing – it’s a game‑changer for patient safety 😊
Jacqui Bryant
February 14, 2026 AT 14:07Agree we should work together to make that happen.