First-Generation Antihistamine Drowsiness Calculator
How Long Will You Be Impaired?
Your Results
Results will appear here after calculation
Many people reach for diphenhydramine - the active ingredient in Benadryl - when they have allergies, a cold, or trouble sleeping. It’s cheap, easy to find, and works fast. But behind that quick relief is a hidden cost: first-generation antihistamines don’t just block histamine. They flood your brain, slow your mind, and dry out your body in ways most users never expect.
What Makes First-Generation Antihistamines Different?
First-generation antihistamines like diphenhydramine, chlorpheniramine, promethazine, and hydroxyzine were developed in the 1940s and 50s. They work by blocking histamine H1 receptors - the same ones that trigger sneezing, itching, and runny noses. But unlike modern versions, these drugs slip easily through the blood-brain barrier. That’s why they’re so effective for sleep and motion sickness - they’re not just acting on your nose or skin. They’re changing how your brain works.
Brain-to-plasma concentration ratios for these drugs range from 1.5:1 to 5:1. That means your brain gets 1.5 to 5 times more of the drug than your blood. Compare that to second-generation antihistamines like cetirizine or loratadine, which stay below 1 ng/mL in the brain even at full doses. That’s the difference between feeling drowsy and feeling normal.
The Drowsiness Isn’t Mild - It’s Dangerous
People often think, “I took Benadryl at night, so I’ll be fine in the morning.” But the drowsiness doesn’t vanish when you wake up. Studies show cognitive impairment from first-generation antihistamines can last up to 18 hours after a single dose. Driving simulators show impairment levels of 0.7 to 0.9 on a scale where 1.0 is maximum intoxication. That’s close to being legally drunk.
According to NHTSA data, 35% of emergency visits for drowsy driving involve these medications. One Reddit user wrote: “Took Benadryl at 8 PM for hives and woke up at 2 PM the next day feeling like I’d been hit by a truck.” That’s not an exaggeration. It’s a documented effect. The FDA warns that diphenhydramine can impair reaction time for six hours - but real-world data shows it’s longer.
And it’s not just driving. People report trouble concentrating at work, forgetting names, mixing up tasks, and feeling mentally foggy all day. In a 2023 survey of 3,782 users on Drugs.com, 38% reported “extreme sleepiness,” and 22% said they couldn’t focus at all.
Anticholinergic Effects: More Than Just a Dry Mouth
These drugs don’t just block histamine. They also bind to muscarinic receptors - the same ones targeted by drugs used to treat overactive bladder or Parkinson’s. That’s why side effects go beyond sleepiness.
Common anticholinergic effects include:
- Blurred vision
- Difficulty urinating or incomplete emptying
- Constipation
- Severe dry mouth (some users report needing artificial saliva)
- Rapid heartbeat
- Confusion and memory lapses
These aren’t minor inconveniences. For older adults, they’re life-altering. The American Geriatrics Society Beers Criteria lists first-generation antihistamines as potentially inappropriate for people over 65. Why? Chronic use increases dementia risk by 54%. That’s not a small risk - it’s a major red flag.
One 2022 survey of 1,204 older adults using low-dose diphenhydramine for sleep found that 65% said it helped them fall asleep - but 42% experienced morning confusion lasting 3 to 4 hours. That’s not restful sleep. That’s chemical sedation with lingering brain fog.

Why Do People Still Use Them?
If they’re so risky, why are they everywhere? Three reasons: price, availability, and perceived effectiveness.
A 24-tablet bottle of generic diphenhydramine costs around $4.99. The same number of cetirizine tablets runs $14.99. For people without insurance or on tight budgets, the savings are tempting. They’re also sold in nearly every pharmacy, gas station, and grocery store. No prescription needed.
And yes - they work fast. Within 15 to 30 minutes, they stop itching and sneezing. They’re also the most effective OTC option for motion sickness and short-term insomnia. For someone on a road trip or lying awake at 2 a.m., that immediate relief is powerful.
But here’s the problem: people use them for things they weren’t meant for. Chronic allergies? Daily sleep aid? That’s where the real danger builds up. The 54% increased dementia risk comes from long-term, repeated exposure - not a single night of use.
Who Should Avoid Them Completely?
Some people should never take first-generation antihistamines:
- Adults over 65 - even low doses carry high risk
- People with glaucoma - they can raise eye pressure
- Those with urinary retention or enlarged prostate - they worsen symptoms
- Anyone taking other anticholinergics - like some antidepressants or bladder meds
- People who drive, operate machinery, or work in safety-sensitive jobs
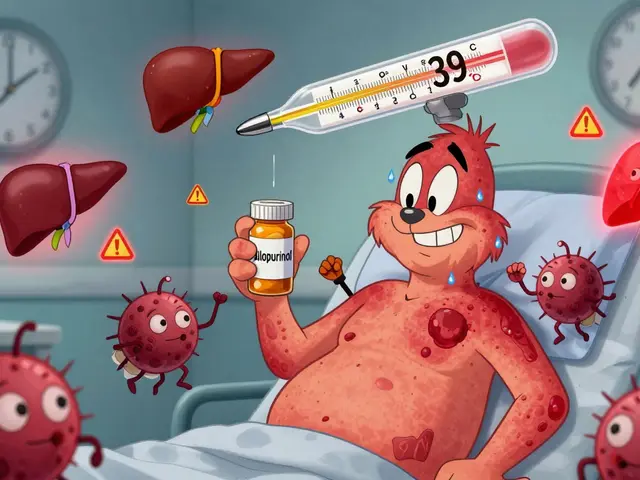
- Anyone with liver disease - they’re metabolized by CYP2D6 and CYP3A4 enzymes, which can be impaired
Even if you’re young and healthy, if you’re taking these daily for allergies, you’re accumulating risk. The brain doesn’t show damage right away. But over years, that anticholinergic burden adds up.

What Are the Better Alternatives?
For allergies, second-generation antihistamines like cetirizine (Zyrtec), loratadine (Claritin), and fexofenadine (Allegra) are safer choices. They don’t cross the blood-brain barrier significantly. You get relief without the fog.
For sleep, melatonin or behavioral changes (like reducing screen time before bed) are more sustainable than diphenhydramine. For motion sickness, ginger or scopolamine patches are more targeted and less sedating.
And for nausea? Metoclopramide or ondansetron are far more effective and don’t carry the same brain risks.
The only time first-generation antihistamines still make sense is for short-term, acute use - like a single night of severe itching or a long car ride. Even then, take the lowest dose possible, avoid alcohol, and never plan to drive or work the next day.
What’s Changing in the Industry?
Regulators are catching up. The UK banned over-the-counter sales of promethazine to minors in 2022. The FDA is considering similar restrictions on diphenhydramine after a 27% spike in pediatric ER visits from misuse between 2018 and 2022.
Pharmaceutical companies are also working on “third-generation” antihistamines. Two candidates, EB-029 and DP-118, are in Phase II trials and show 80% less brain penetration while keeping the same allergy-fighting power. These could be game-changers - if they get approved.
Meanwhile, the FDA now requires stronger labeling on packaging about next-day impairment. But many OTC boxes still downplay the risks. A 2022 JAMA Internal Medicine study found 45% of users underestimated how long the drowsiness would last.
How to Use Them Safely (If You Must)
If you’re going to use a first-generation antihistamine, follow these rules:
- Take it only at night - never during the day.
- Start with half the dose (e.g., 12.5 mg of diphenhydramine) to test your sensitivity.
- Avoid alcohol completely - it doubles the sedative effect.
- Don’t use it for more than 3 to 5 days in a row.
- Never use it as a long-term sleep aid or allergy treatment.
- Check all other medications - many cold, flu, and sleep aids contain hidden first-gen antihistamines.
If you’ve been using these regularly for months or years, talk to your doctor. There are safer options. You don’t have to live with brain fog just to get a good night’s sleep or stop sneezing.
Are first-generation antihistamines safe for older adults?
No. The American Geriatrics Society strongly advises against their use in adults over 65. These drugs increase the risk of cognitive decline, confusion, falls, and dementia by 54% with long-term use. Even low doses can cause lasting brain changes. Safer alternatives like melatonin or non-sedating antihistamines should be used instead.
How long does drowsiness from Benadryl last?
Drowsiness can last 6 to 18 hours after a single dose, depending on metabolism, age, and liver function. Driving simulators show impairment lasting up to 18 hours - longer than many people realize. This is why many users feel foggy the next day, even after a full night’s sleep.
Can first-generation antihistamines cause urinary problems?
Yes. These drugs block muscarinic receptors in the bladder, making it harder to start urinating or fully empty the bladder. This is especially dangerous for men with enlarged prostates and can lead to urinary retention - a medical emergency. Around 28% of long-term users on forums report this issue.
Is it safe to take diphenhydramine every night for sleep?
No. Using diphenhydramine nightly leads to tolerance - you need more to get the same effect - and increases anticholinergic burden. It doesn’t improve sleep quality, only induces chemical sedation. Over time, it can impair memory and increase dementia risk. Better options include sleep hygiene, melatonin, or cognitive behavioral therapy for insomnia (CBT-I).
Do second-generation antihistamines work as well as first-generation ones?
For allergies, yes - and often better. Second-generation antihistamines like cetirizine and loratadine are just as effective at stopping sneezing and itching, but without the drowsiness or cognitive fog. They’re longer-lasting (12-24 hours), so you take them once a day. The only exceptions are motion sickness and acute insomnia, where first-gen drugs still have an edge.
What should I do if I’ve been taking Benadryl daily for years?
Talk to your doctor or pharmacist. Don’t stop abruptly - especially if you’ve been using it for sleep. Ask about switching to a non-sedating antihistamine for allergies or exploring non-drug options for sleep. Your long-term brain health matters more than the convenience of a quick fix.




Jennifer Anderson
December 6, 2025 AT 18:23so i just took benadryl last night for my hives and woke up feeling like my brain was wrapped in wet cardboard 😅
Helen Maples
December 7, 2025 AT 11:13The data is unequivocal: first-generation antihistamines are neurotoxic with chronic use. The 54% increased dementia risk isn't a statistical fluke-it's a pharmacological inevitability. Regulatory bodies are slow, but the science is clear. Stop normalizing chemical sedation as self-care.
Sadie Nastor
December 9, 2025 AT 01:11i feel you, helen. i used to take it every night for years thinking it was 'natural sleep'... then i realized i was forgetting where i put my keys every day. switched to melatonin and my brain feels like it's been let out of jail 🙏
Kyle Flores
December 10, 2025 AT 20:52my grandma took diphenhydramine for 15 years. she started forgetting names, then her own birthday. by 82, she was diagnosed with early-onset dementia. the doctor said it was likely from years of anticholinergic burden. i wish someone had told us sooner.
Nancy Carlsen
December 11, 2025 AT 04:16my mom is 70 and still takes it for 'sleep'. i showed her the Beers Criteria and she cried. she said she didn't know it was hurting her brain. we switched her to magnesium glycinate and she's sleeping better now. please, if you're over 65, talk to your pharmacist. they know more than you think 💛
Ted Rosenwasser
December 12, 2025 AT 22:06Let’s be real-this is just another fearmongering piece from the pharmaceutical-industrial complex trying to sell you $15 Zyrtec. Benadryl’s been around for 70 years. If it were that dangerous, wouldn’t we all be dead by now? Also, your 'second-gen' drugs are just rebranded generics with a premium price tag. Wake up.
Ashley Farmer
December 13, 2025 AT 23:10i know people who use this daily and don’t realize how foggy they are. i work with someone who calls me three times a day asking the same question. she says she's 'just tired'-but she takes benadryl for allergies. she doesn't even know she's impaired. it's scary how normal it's become.
David Brooks
December 15, 2025 AT 08:36I took Benadryl for a flight last year. Woke up 12 hours later in a hotel room with no memory of checking in. My phone was on airplane mode, my wallet was in the fridge, and I had a half-eaten bag of pretzels in my lap. That’s not sleep. That’s a chemical blackout. Never again.
Olivia Hand
December 15, 2025 AT 23:33It’s not just about cognition-it’s about autonomy. When you’re drugged into sleep, you’re surrendering your neurological sovereignty to a $5 bottle of pills. That’s not rest. That’s surrender. And we’re raising a generation that thinks chemical sedation is the price of adulting. We need better.
Kyle Oksten
December 17, 2025 AT 12:53What’s the alternative? To suffer through hay fever or insomnia? Society doesn’t provide real solutions-just marketing. People take Benadryl because they’re exhausted, overworked, and have no access to proper care. Blaming the drug ignores the system that made it necessary.
Ernie Blevins
December 19, 2025 AT 06:39they put this stuff in everything. cough syrup, sleep aids, even some painkillers. you think you're safe because you only take it 'when needed'? nah. you're getting it every day without knowing. big pharma wants you addicted to brain fog.
Stacy here
December 19, 2025 AT 06:57They’re hiding the truth. The FDA banned it in the UK for minors because they know it’s a mind-control agent. They’re slowly drugging the population so we don’t question the system. Wake up. This isn’t medicine-it’s population management. The 'dementia risk' is just a cover for the real agenda.
Sam Mathew Cheriyan
December 20, 2025 AT 14:51bro in india we use it for everything. cold, sleep, even stomach pain. my uncle took it for 20 years and now he can’t walk straight. but he says it’s fine. what do i know? i’m just a guy with internet.
Nicholas Heer
December 21, 2025 AT 19:04the government doesn't want you to know this. why? because if you stop taking benadryl, you'll start asking why your job makes you so tired. why your healthcare costs so much. why you're not allowed to sleep without a pill. they profit from your fog. don't be their zombie.
Sangram Lavte
December 21, 2025 AT 21:56i used to take it for allergies. switched to loratadine. no drowsiness, same relief. cost difference? $10 a month. worth every penny. your brain is not a sacrifice zone.