Fluoroquinolone Tendon Risk Calculator
This calculator estimates your risk of tendon injury when taking fluoroquinolone antibiotics based on key factors. Always consult your doctor before making treatment decisions.
Your Risk Factors
Your Risk Assessment
Fluoroquinolones are powerful antibiotics. They treat serious infections like pneumonia, complicated urinary tract infections, and even anthrax. But for some people, they come with a dangerous hidden cost: tendon rupture. It’s not a rare side effect. It’s not a footnote. It’s a real, documented risk that can turn a simple course of antibiotics into a life-altering injury.
Which Fluoroquinolones Carry the Highest Risk?
Not all fluoroquinolones are created equal when it comes to tendon damage. The data shows clear patterns. Levofloxacin is the most frequently linked to tendon problems, appearing in over half of reported cases. Ciprofloxacin comes in second, responsible for nearly 40% of cases. Moxifloxacin, though less common, still carries significant risk. These three make up over 93% of fluoroquinolone-related tendon injuries tracked globally.
The Achilles tendon - the thick cord connecting your calf muscle to your heel - is the most vulnerable. Studies show it’s involved in nearly 90% of cases. But it’s not alone. Tendons in the shoulder, hand, and rotator cuff can also be affected. And in about half of all cases, both sides of the body are injured at once.
How Fast Can This Happen?
Most people assume side effects show up after weeks. Not with fluoroquinolones. The median time from starting the drug to first signs of tendon pain? Just six days. Eighty-five percent of cases develop within the first month. And here’s the scary part: symptoms can appear as early as 48 hours after your first pill. One documented case showed tendon pain starting just two hours after taking the medication.
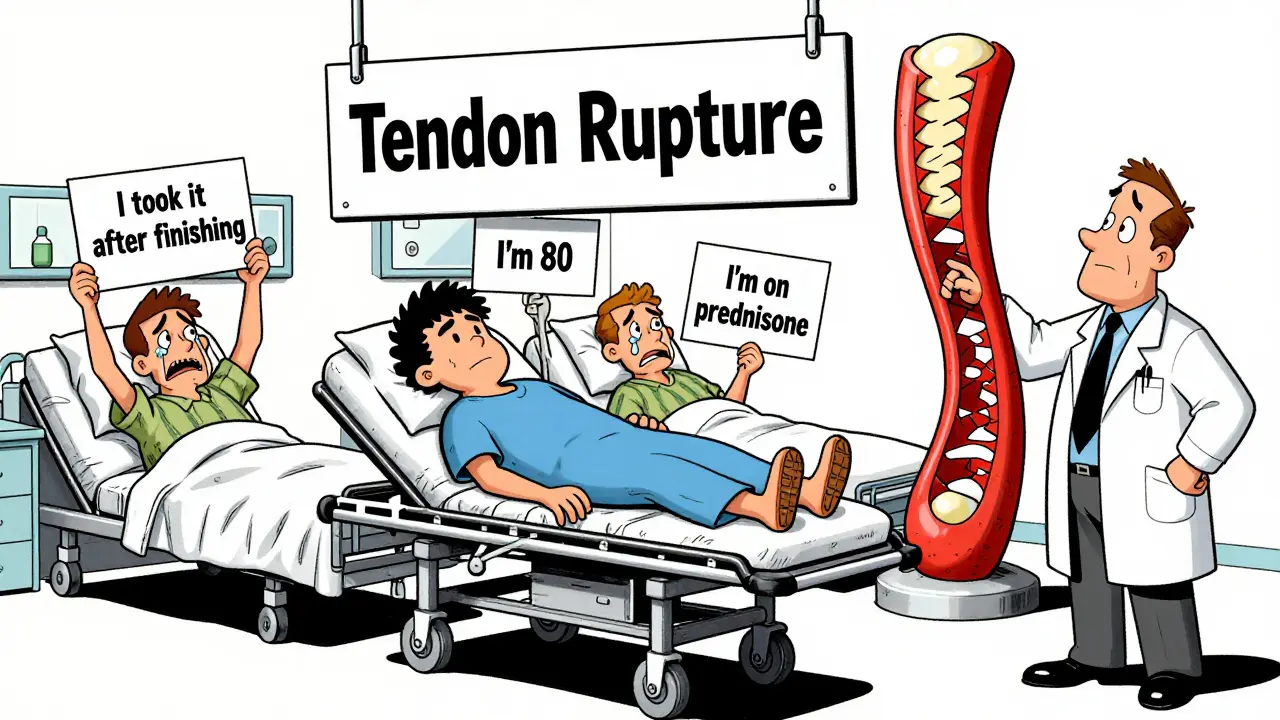
And it doesn’t stop when you finish the course. Up to half of tendon injuries occur after you’ve stopped taking the antibiotic. That means you could feel fine for weeks, then suddenly wake up with sharp pain in your heel or shoulder. The damage is already done.
Who’s Most at Risk?
This isn’t a risk that affects everyone equally. Certain people face dramatically higher chances of tendon rupture.
- Age 60 and older: Your risk jumps 6.4 times if you’re between 60 and 79. If you’re 80 or older? The risk skyrockets to 20 times higher than younger adults.
- On corticosteroids: This is the biggest red flag. Taking prednisone, methylprednisolone, or any steroid - even a short course - increases your rupture risk by 46 times. That’s not a typo. It’s a medical emergency waiting to happen.
- Diabetes or kidney disease: Both conditions impair tissue repair and increase oxidative stress. If you have either, your body can’t recover from the cellular damage fluoroquinolones cause.
- History of tendon problems: If you’ve had tendinitis before, especially from exercise or injury, you’re far more likely to have it again with these antibiotics.
Women also appear to have a slightly higher association with tendonitis and rupture than men, though the reason isn’t fully understood. It may relate to hormonal differences in collagen structure or how the body processes these drugs.

Why Do Fluoroquinolones Damage Tendons?
It’s not just an allergy or a random glitch. Fluoroquinolones attack tendons at the cellular level. They interfere with mitochondria - the energy factories inside your cells. This causes oxidative stress, a buildup of toxic molecules that break down collagen, the main structural protein in tendons.
They also block an enzyme called topoisomerase II, which helps cells repair DNA. Tendon cells are slow to regenerate, so this interference leaves them vulnerable. Plus, fluoroquinolones bind to magnesium and calcium - minerals your tendons need to stay flexible and strong. Without them, tendons become brittle.
Think of it like rust on a steel cable. The antibiotic doesn’t cut the cable. It slowly weakens it from the inside until one simple movement - a step, a sneeze, lifting a grocery bag - snaps it clean in two.
What Does the Evidence Say?
Large studies confirm the danger. A UK analysis of 6.4 million patients found fluoroquinolone users were 4.3 times more likely to develop tendinitis and twice as likely to suffer a full rupture. In Taiwan, a study of over 350,000 people showed fluoroquinolone users had nearly double the rate of tendon disorders compared to those who didn’t take them.
But not all studies agree. A 2022 Japanese study of 504 patients found no significant link between fluoroquinolones and tendon rupture. Why? Possibly because their population was younger, had fewer comorbidities, or used different dosing patterns. This contradiction doesn’t mean the risk is fake - it means the risk isn’t uniform. For some, it’s low. For others, it’s catastrophic.
Regulatory agencies haven’t ignored this. The FDA added a black-box warning in 2008 - their strongest possible alert. The UK’s MHRA and Europe’s EMA followed with strict prescribing rules. These drugs are no longer first-line treatments. They’re reserved for life-threatening infections when nothing else works.
What Should You Do?
If you’re prescribed a fluoroquinolone, ask these questions:
- Is this infection truly life-threatening? Or can another antibiotic do the job?
- Am I over 60? Do I take steroids? Do I have diabetes or kidney issues?
- What are the signs of early tendon damage? (Pain, swelling, stiffness - especially in the heel or shoulder.)
- What happens if I stop the drug at the first sign of pain?
Don’t wait for a rupture. If you feel sudden tendon pain - even mild - stop the medication immediately and call your doctor. Don’t assume it’s just muscle soreness. Early intervention can prevent a complete tear. Immobilizing the area and switching to a safer antibiotic can save you from surgery, months of rehab, or permanent disability.
Alternatives Exist
For most common infections - sinusitis, bronchitis, simple UTIs - there are better choices. Amoxicillin, doxycycline, nitrofurantoin, and trimethoprim-sulfamethoxazole are effective and carry far less risk of tendon damage. Fluoroquinolones should only be used when those options have failed or aren’t suitable.
The Infectious Diseases Society of America now recommends reserving fluoroquinolones as third-line therapy. That means try two safer options first. If those don’t work, then consider this one - with full awareness of the risks.
Final Reality Check
Over 25 million fluoroquinolone prescriptions are written in the U.S. every year. That’s a lot of people exposed to this risk. Many take them without knowing the danger. But the data is clear: tendon rupture isn’t a myth. It’s a real, preventable injury.
If you’re older, on steroids, or have chronic health issues, this isn’t just a warning. It’s a red alert. Talk to your doctor. Ask for alternatives. Don’t let convenience override safety. One pill might save you from infection. But it could also end your ability to walk, climb stairs, or lift your child.
Can fluoroquinolones cause tendon damage even after I stop taking them?
Yes. While most tendon issues start within the first month of use, up to 50% of cases occur after the medication has been stopped. The damage can develop slowly, and symptoms like pain or stiffness may appear weeks later. This makes it harder to connect the injury to the antibiotic, which is why doctors stress immediate reporting of any new tendon pain - even after finishing the course.
Is tendon rupture from fluoroquinolones reversible?
It depends. Mild tendinitis may improve with rest, physical therapy, and stopping the drug. But once a tendon ruptures completely, surgery is almost always required. Even after repair, many patients experience lasting weakness, reduced mobility, or chronic pain. Some never fully recover their previous level of function. That’s why prevention is critical - not treatment.
Are there any safe fluoroquinolones?
No. All fluoroquinolones carry the same class-wide risk of tendon damage. While some, like levofloxacin and ciprofloxacin, are more commonly reported in cases, no fluoroquinolone is considered safe for tendon health. The risk is inherent to the chemical structure of this entire antibiotic class.
Why is the Achilles tendon most often affected?
The Achilles tendon is under constant mechanical stress and has relatively poor blood supply, making it slower to repair itself. Fluoroquinolones reduce collagen strength and impair healing, which hits tendons with low blood flow the hardest. The Achilles also bears the full weight of the body during walking and running, increasing strain. This combination makes it the most vulnerable.
Should I avoid fluoroquinolones if I’m active or exercise regularly?
Yes, especially if you’re over 50 or have other risk factors. Exercise increases tendon load, and fluoroquinolones weaken tendon structure. The combination raises the chance of rupture during normal activity - not just injury. Even light jogging or stair climbing can trigger a rupture in someone on these drugs. If you’re active, ask your doctor for a non-fluoroquinolone alternative.