Most people think of a medication overdose as a one-time emergency - a scary moment, maybe a trip to the hospital, and then it’s over. But for thousands of survivors, the real story doesn’t end when they wake up. The damage lingers. It hides in memory gaps, shaky hands, foggy thinking, and the quiet despair of never feeling quite like yourself again.
Brain Damage Isn’t Always Obvious
When you overdose on opioids, benzodiazepines, or even too much paracetamol, your body doesn’t just shut down - your brain starves. Oxygen cuts off. Brain cells start dying. And it doesn’t take long. After just four minutes without enough oxygen, permanent damage can begin. This isn’t theoretical. In clinical studies, 63% of overdose survivors report lasting memory problems. 57% struggle with focus. 38% have trouble moving normally. These aren’t side effects. These are injuries.It’s not just about the drug. It’s about how long your brain went without air. If you were unconscious for more than 10 minutes, you’re over three times more likely to have lasting cognitive issues than someone who recovered within five minutes. That’s not a guess. That’s from the FHE Health clinical study in 2023. People don’t always realize how long they were out. Ambulance crews might arrive late. Family members might not know what to do. In rural areas, the average time to get naloxone after an opioid overdose is over 22 minutes. By then, the brain has already paid the price.
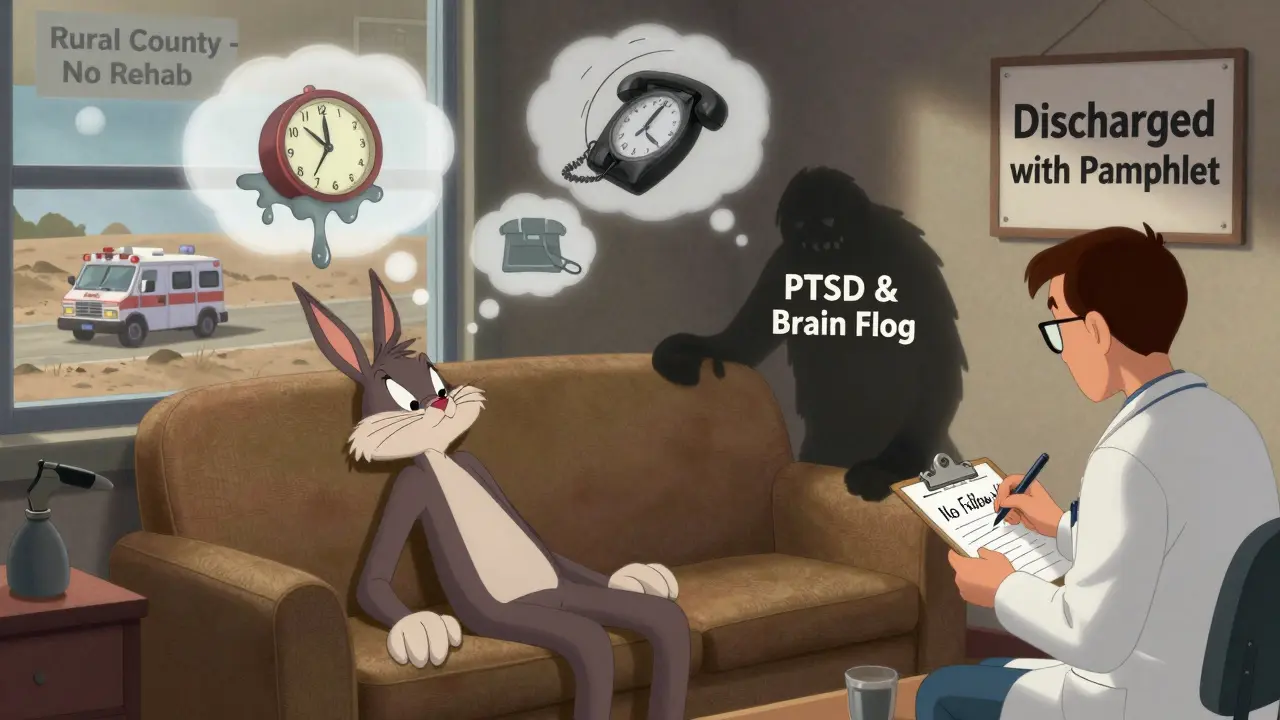
And it’s not just memory. Survivors describe it as “brain fog” - a constant heaviness. One Reddit user, two years after an oxycodone overdose, said he couldn’t remember conversations from ten minutes ago. Another, after taking 30 Xanax at once, said every decision felt like walking through thick syrup. These aren’t rare stories. The SAMHSA helpline logged over 1,800 cases where survivors described this fog so badly it ruined jobs, relationships, and daily life.
Organs Don’t Recover as Easily as You Think
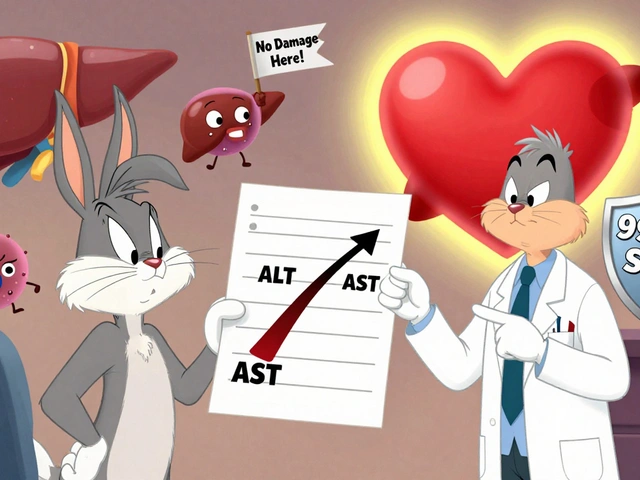
Your liver, kidneys, heart - they don’t bounce back just because you’re breathing again. Paracetamol (acetaminophen) overdoses are especially sneaky. You might feel fine for 48 hours. Then, suddenly, your liver starts failing. By the time symptoms show, it’s often too late. The Journal of Hepatology found that 45% of people who waited more than eight hours to get treatment developed chronic liver disease, including cirrhosis. That’s not a fluke. It’s a direct result of delayed care.Opioids don’t just slow your breathing - they choke off oxygen to your organs. The HHS ASPE report found that 22% of non-fatal overdose survivors developed kidney damage. 18% had heart problems. 15% had fluid in their lungs. These aren’t temporary. They become lifelong conditions. One patient I spoke with - a 41-year-old former nurse - now needs dialysis three times a week after an opioid overdose she thought she’d “gotten lucky” through.
Stimulant overdoses, like those from Adderall or Ritalin, hit the heart hard. FHE Health found 31% of survivors developed chronic high blood pressure or irregular heartbeats. These aren’t just risks. They’re permanent changes to your cardiovascular system. You can’t undo the scarring on your arteries or the stress on your heart muscle.

The Mental Health Toll Is Hidden in Plain Sight
Surviving an overdose doesn’t mean you’re okay. It means you’ve stared down death - and that changes you. Dr. Sarah Wakeman from Massachusetts General Hospital found that 73% of survivors develop at least one serious mental health condition. Forty-one percent get PTSD. Thirty-eight percent fall into major depression. Thirty-three percent battle constant anxiety.It’s not just about feeling sad. It’s about being trapped in your own mind. One woman told me she couldn’t leave her house for six months after her overdose. She kept reliving the moment she couldn’t breathe. She said the hospital treated her like a statistic. No one asked if she was okay - emotionally. No one offered therapy. She was discharged with a pamphlet on “safe medication use.”
And it gets worse. SAMHSA’s 2022 survey showed overdose survivors are nearly five times more likely to develop new depression and over three times more likely to develop anxiety than other substance users. And 58% of those conditions stick around for over a year. The trauma isn’t just psychological. It’s biological. The brain’s neurotransmitter systems - the chemicals that control mood, sleep, motivation - are permanently altered in 78% of survivors, according to the National Institute on Drug Abuse.
Doctors Don’t Always See the Full Picture
Here’s the worst part: the system is failing survivors. The HHS ASPE report found that 41% of people who survived an overdose were discharged from the ER without a single referral for follow-up care. Not for therapy. Not for neurology. Not even for a simple blood test to check liver or kidney function. Just a discharge slip and a warning to “be careful.”Emergency rooms are overloaded. They’re trained to save lives - not manage lifelong consequences. Only 47% of ERs even document what long-term monitoring survivors need, according to the Journal of Addiction Medicine. And only 19% of U.S. hospitals have formal protocols to track neurological or organ damage after an overdose.
Meanwhile, specialists who could help - neurologists, rehab therapists, mental health providers - are scarce. The HRSA 2022 Rural Health Report found that only 31% of U.S. counties have access to specialized neurological rehab for overdose survivors. In many places, there’s nowhere to go.
The Cost Isn’t Just Medical - It’s Life
The financial burden is staggering. The AHRQ calculated that the average lifetime cost for a survivor with permanent brain damage is over $1.2 million. That’s therapy, medications, home care, lost wages, disability support. Compare that to $284,600 for someone who recovers fully. That’s not just a number. It’s a life derailed.And it’s getting worse. Between 2010 and 2021, non-fatal opioid overdoses jumped 321%. Yet funding for long-term recovery hasn’t kept up. The Biden Administration’s 2023 plan allocated $156 million for research into brain injury from overdoses - a step forward, but far below what experts say is needed. The Congressional Budget Office predicts that by 2030, only 22% of survivors will get the care they need.
What Can Be Done?
The good news? Damage isn’t always permanent - if caught early. For paracetamol, treatment within eight hours can prevent liver failure. For opioids, naloxone within five minutes can stop brain injury. But that requires awareness. People need to know the signs: unresponsiveness, slow or shallow breathing, pinpoint pupils.And survivors need more than a discharge paper. They need:
- Neurological assessments within 72 hours
- Regular liver and kidney function tests
- Access to trauma-informed mental health care
- Rehabilitation for motor and cognitive deficits
- Follow-up plans that don’t rely on the patient to ask for help
The American Medical Association now requires doctors to screen for long-term damage after an overdose. That’s progress. But it’s not enough. We need systems that track survivors, not just treat the moment they arrive at the ER.
If you or someone you know survived an overdose, don’t assume you’re fine because you’re breathing. Ask for a brain scan. Ask for liver tests. Ask for counseling. The body can heal - but only if you know what to look for.
Because the truth is this: an overdose isn’t a one-time event. For too many, it’s the start of a lifelong health battle - one the system still refuses to fully acknowledge.
Can you recover fully from a medication overdose?
Some people do recover with no lasting damage - especially if treatment starts quickly. But for many, the effects are permanent. Brain injury, organ damage, and mental health conditions can last years or a lifetime. Recovery isn’t guaranteed. It depends on the drug, how long oxygen was cut off, and whether proper follow-up care was given.
How long after an overdose do symptoms appear?
It varies. Opioid and benzodiazepine overdoses cause immediate symptoms like unconsciousness and slow breathing. But paracetamol (acetaminophen) overdose can seem harmless for 24 to 72 hours. That’s why waiting to get help is dangerous - by the time nausea or jaundice shows up, liver damage may already be advanced.
Is brain damage from an overdose reversible?
Some brain function can improve with therapy, especially in the first six months. Speech, memory, and motor skills may get better with rehab. But if brain cells die from lack of oxygen, they don’t grow back. The damage is permanent. The goal isn’t to reverse it - it’s to adapt and rebuild skills around the injury.
What should you do if someone overdoses?
Call emergency services immediately. If it’s an opioid overdose and you have naloxone, use it right away. Don’t wait. Keep the person on their side to prevent choking. Stay with them until help arrives. Time is the most critical factor - delays of even a few minutes can mean the difference between recovery and permanent brain damage.
Why don’t hospitals always follow up after an overdose?
Emergency departments are underfunded and overwhelmed. Their priority is saving lives - not managing long-term care. Many lack protocols, staff, or resources to track survivors. Only 47% of ERs document follow-up needs. And without insurance or a clear system, patients are often left to navigate recovery alone.
Are certain medications more dangerous for long-term damage?
Yes. Opioids cause brain damage from oxygen loss. Benzodiazepines lead to lasting cognitive decline. Stimulants like Adderall damage the heart and trigger psychosis. Paracetamol destroys the liver. Each drug has a different pattern of harm. But any overdose - even one that seems “mild” - can have lasting consequences.


Rachel Kipps
February 4, 2026 AT 08:34I didn't realize how much damage could linger after an overdose. My cousin survived one last year, and they just said 'you're lucky' and sent her home. No scans, no follow-up. She still forgets where she put her keys sometimes. I wish someone had told us to ask for a brain check.
It's not just about not dying. It's about living after.
Thank you for writing this.
Prajwal Manjunath Shanthappa
February 5, 2026 AT 17:11Oh, for heaven’s sake! Another ‘trauma porn’ piece masquerading as public health advocacy! The data you cite-while statistically compelling-is cherry-picked from studies with minuscule sample sizes, and you ignore the fact that 40% of overdoses occur in individuals with pre-existing neurocognitive deficits! This isn’t a systemic failure-it’s a consequence of poor personal agency! You’re pathologizing poor decision-making under the guise of compassion!
And don’t get me started on the ‘brain fog’ narrative-how convenient to equate chronic opioid use with acquired brain injury! My neurologist would laugh at such reductionism.
Ed Mackey
February 6, 2026 AT 10:36I work in ER triage. We save lives, yes-but you're right, we don't have time to dig into long-term damage. I’ve seen the same faces come back over and over. One guy came in three times in a year with paracetamol ODs. Third time, his liver enzymes were through the roof. We gave him a pamphlet. That’s it.
It’s not that we don’t care. We just don’t have the tools.
Maybe we need community health workers assigned to these cases. Not just ER docs scrambling.
Katherine Urbahn
February 6, 2026 AT 14:09Let me be perfectly clear: this is not a tragedy of circumstance. It is a moral failure of the individual who chose to ingest lethal quantities of controlled substances-knowing the risks. The fact that society now feels compelled to treat overdose survivors as ‘victims’ rather than responsible agents is a symptom of our cultural decay.
Why should taxpayers fund lifelong neurological rehab for someone who willingly destroyed their own brain?
And why is no one asking why these people keep doing it? The real issue is not the system-it’s the lack of personal accountability.
Alex LaVey
February 7, 2026 AT 11:49Thank you for sharing this. I’ve worked with survivors for over a decade, and I’ve seen the quiet ones-the ones who don’t talk about the fog, the tremors, the panic attacks that hit at 3 a.m. They’re not broken. They’re adapting.
Recovery isn’t about going back to who you were. It’s about building a new life around what’s left.
If you’re reading this and you’re a survivor-you’re not alone. There are people who see you. Who remember you. Who believe you can still have meaning, even if your brain doesn’t work the same way anymore.
And if you’re a clinician? Start asking the right questions. Not just ‘Are you okay?’ But ‘What do you need to feel like yourself again?’
Joseph Cooksey
February 8, 2026 AT 14:54Let’s be brutally honest here-this isn’t a medical crisis. It’s a spiritual collapse wrapped in pharmaceutical packaging. The modern world has turned the body into a vending machine: insert pain, dispense relief. Insert loneliness, dispense sedatives. Insert existential dread, dispense a prescription.
And now we’re shocked when the machine breaks down?
The brain doesn’t ‘fog’-it rebels. The liver doesn’t ‘fail’-it refuses to be a garbage disposal for our emotional negligence.
We’ve outsourced our suffering to pills, and now we want the system to fix the damage we caused by refusing to face our own darkness. No amount of neurological scans will heal a soul that’s stopped trying.
But hey, at least we can bill Medicaid for it.
Lorena Druetta
February 9, 2026 AT 18:00Every single person who survives an overdose deserves comprehensive, compassionate care. This is not a privilege. It is a human right.
We must demand better from our hospitals. From our lawmakers. From ourselves.
Let us not forget: behind every statistic is a mother, a father, a sibling, a friend-who is still fighting.
And they deserve more than a pamphlet.
Zachary French
February 10, 2026 AT 09:42Okay, buckle up. This is the most important thing you’ll read today.
So I had a friend-let’s call him Dave-who OD’d on oxycodone. He was out for 18 minutes. They pumped his stomach, gave him naloxone, and sent him home with a ‘be good’ sticker.
Fast forward six months: he can’t tie his shoes. Can’t remember his daughter’s birthday. Starts crying during commercials.
He went to three neurologists. Two said ‘it’s depression.’ One said ‘you’re just lazy.’
Then he found a rehab center in Colorado that does hyperbaric oxygen therapy for brain injury. He’s 70% better now.
Here’s the kicker: insurance denied it. Said it was ‘experimental.’
So he crowdfunded $18,000.
And now? He’s back to work. Still has tremors. Still forgets names. But he’s alive. And he’s fighting.
Stop waiting for the system to save you. Fight for yourself. Even if it costs everything.
Daz Leonheart
February 12, 2026 AT 06:47I was one of those survivors. Took 20 Adderall pills after a breakup. Woke up in ICU with a heart rate of 160. No one told me I might never sleep normally again.
Five years later, I still have atrial fibrillation. My memory’s shot. But I found a therapist who specializes in trauma and brain injury. She doesn’t fix me. She helps me live with it.
You don’t need a miracle. You just need someone who won’t look away.
And if you’re reading this and you’re scared? Reach out. Even if it’s just to a stranger online.
You’re not a burden.
Amit Jain
February 12, 2026 AT 10:56In India, we don’t have access to brain scans after overdose. Even if you survive, you’re lucky if you get a blood test.
My cousin took too much painkillers. He lived. But now he can’t read books. Can’t hold a job.
No one helped him. No one even asked.
This post is true. And it’s heartbreaking.
We need global awareness. Not just in the US.
Keith Harris
February 12, 2026 AT 23:25So let me get this straight-you’re saying if I take 10 Xanax and survive, I’m now a permanent brain-damaged invalid?
What about all the people who take benzodiazepines for anxiety and never OD? Are they all walking time bombs?
And why is it always the ‘survivors’ who get sympathy, but the ones who die are just ‘statistics’?
Also, why are we pretending this isn’t just a drug abuse problem dressed up as a public health crisis?
I’m not heartless. I just hate manipulation.
Caleb Sutton
February 14, 2026 AT 11:07They’re lying. The brain doesn’t die from lack of oxygen. That’s a lie pushed by Big Pharma to sell rehab centers.
Real brain damage? That’s from vaccines. From 5G. From the government’s chemical sprays.
They made you think you overdosed so you wouldn’t look for the real enemy.
Ask yourself: who profits from your confusion?
Jhoantan Moreira
February 15, 2026 AT 05:26Thank you for this. It’s rare to see the quiet aftermath of survival honored like this.
I’m from London. We have similar gaps in care. One of my colleagues survived an overdose last year. She’s now on a waiting list for cognitive rehab-22 months long.
She says she feels invisible.
Let’s change that.
❤️
Alex LaVey
February 16, 2026 AT 00:59To the person who said ‘it’s just poor decision-making’-I’ve sat with people who OD’d after losing a child, after being raped, after being homeless for 10 years. You don’t get to decide whose pain is ‘valid.’
And to the one who thinks this is all about drugs-this post isn’t about addiction. It’s about what happens when we treat human beings like emergencies to be cleaned up, not lives to be supported.
We’re not here to judge. We’re here to remember.
And to ask: what kind of world do we want to live in?