What if your pain isn’t telling you your body is broken?
For years, people with chronic pain were told their discomfort came from damaged tissues-worn-out discs, torn ligaments, arthritic joints. Doctors pointed to X-rays and MRIs like they were crime scene photos. But here’s the truth: pain doesn’t always match up with what’s happening in your body. You can have severe pain with no visible damage. And you can have major structural changes with zero pain. That’s not a mistake. It’s biology.
Pain Neuroscience Education (PNE) flips the script. Instead of treating pain like a signal from a broken machine, it teaches you that pain is your brain’s protective alarm. Sometimes that alarm gets too sensitive. It goes off even when there’s no fire. PNE helps you understand why that happens-and how to turn it down.
How pain really works (no jargon, just facts)
Your nerves don’t send pain signals like a phone call saying, “My back is broken!” They send danger signals-lots of them. Your brain collects all those signals, plus your mood, your stress levels, your past experiences, even what you’ve been told about pain. Then it decides: “Is this a real threat?” If it thinks yes, you feel pain. If it thinks no, you might feel nothing at all.
This is called the neuromatrix model. It’s not just nerves and bones. It’s your whole system working together. When pain lasts longer than three months, your nervous system starts to change. This is called central sensitization. Your brain and spinal cord become more responsive. Even light touches can feel painful. A breeze on your skin might trigger a flare-up. That’s not because you’re worse-it’s because your alarm system is stuck on high volume.
Think of it like a smoke alarm that goes off every time you burn toast. Over time, it starts going off for steam, for dust, for your shadow. The alarm isn’t broken. It’s just too sensitive. PNE helps you retrain that alarm.
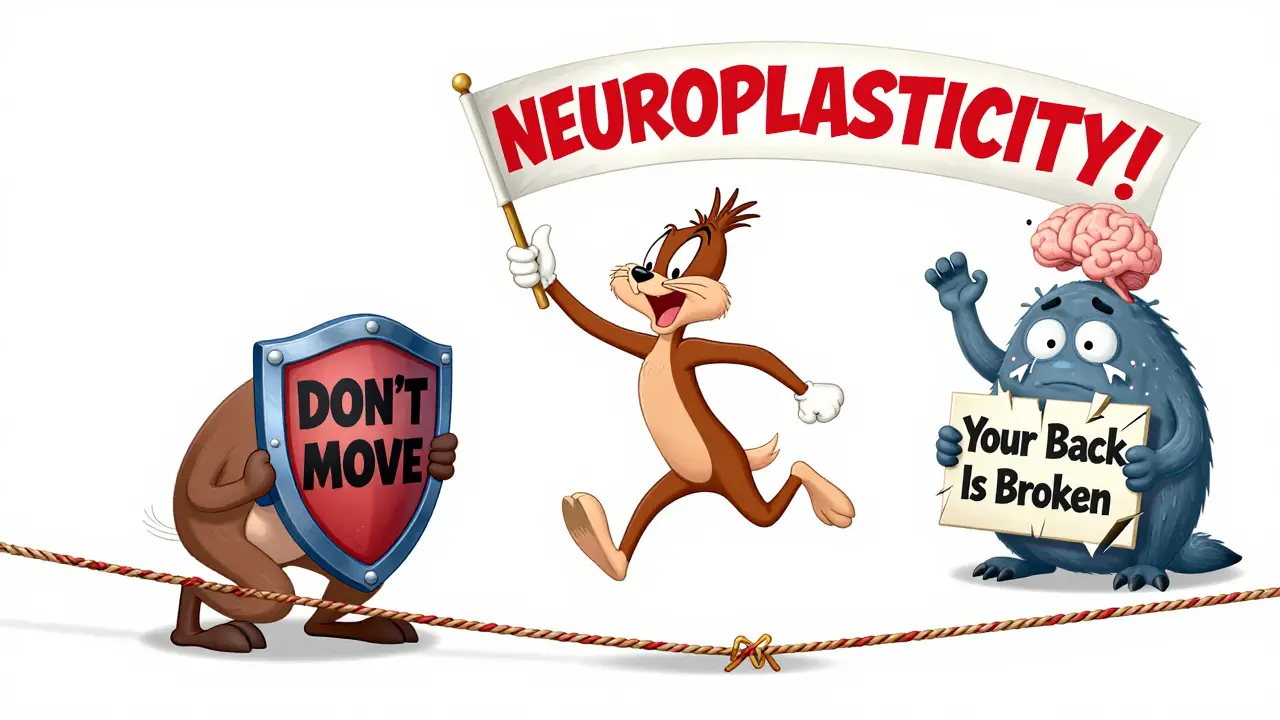
Why traditional pain advice often makes things worse
Most people with chronic pain are told to rest, avoid movement, and fear certain activities. “Don’t lift that.” “Don’t bend over.” “Your spine is fragile.” These messages might sound caring, but they teach your brain that your body is dangerous. And that makes pain worse.
A 2023 review of 23 studies found that patients who were told to avoid movement showed higher levels of pain catastrophizing-a mindset where pain feels overwhelming, uncontrollable, and terrifying. That mental state actually increases pain signals in the brain. It’s a loop: fear → avoidance → stiffness → more pain → more fear.
PNE breaks that loop. Instead of saying “Your back is damaged,” it says, “Your nervous system is overreacting.” That small shift changes everything. Suddenly, movement isn’t a threat. It’s a way to calm your alarm.
What happens in a typical PNE session
PNE isn’t a lecture. It’s a conversation. A trained therapist-usually a physical therapist, sometimes a psychologist or doctor-uses simple metaphors and visuals to explain pain biology. One common metaphor is the “smoke alarm.” Another is the “alarm system” in your brain that’s been turned up too high.
Sessions last 30 to 45 minutes. They’re usually done one-on-one, though group sessions are growing in popularity. The goal isn’t to make you pain-free overnight. It’s to help you understand why you feel pain the way you do. After a few sessions, patients often say things like, “I thought I was broken. Now I realize my body is just scared.”
Studies show that after PNE, people report:
- A drop of 1.7 points on a 0-10 pain scale
- A 20% improvement in daily function
- A 6-point drop in pain catastrophizing scores
Those numbers might seem small, but in real life, they mean you can pick up your grandchild again. Walk to the shop without dreading it. Sleep through the night. That’s not magic. That’s neuroscience.
PNE works best with movement-not instead of it
PNE alone helps. But it shines when paired with gentle movement or exercise. One study found that when PNE was combined with physical activity, pain improved by 30-40% more than with either approach alone.
Why? Because movement teaches your brain safety. When you slowly bend, reach, or walk without pain flaring up, your brain learns: “This isn’t dangerous.” That’s called neuroplasticity-your brain rewiring itself based on new experiences.
Think of it like learning to ride a bike. At first, you’re scared you’ll fall. But every time you get back on, your fear shrinks. PNE gives you the knowledge. Movement gives you the proof.
Who benefits most-and who doesn’t
PNE works best for people with chronic pain lasting more than three months. That includes low back pain, fibromyalgia, chronic neck pain, and complex regional pain syndrome. In 82% of studies, patients with long-term pain saw real improvements.
It’s less helpful for acute pain-like after surgery or a sprained ankle-where tissue damage is clearly the main issue. One review found only 11% of acute pain cases showed benefit from PNE.
It also doesn’t work well for people with severe cognitive impairment or very low health literacy. If someone can’t follow a story about an alarm system, complex brain science won’t help. That’s why good practitioners adapt: they use simpler language like “your body’s alarm is too loud” instead of “central sensitization.”
And PNE won’t help if you expect it to make your pain vanish. It’s not a cure. It’s a shift in understanding. If you’re looking for a magic pill, you’ll walk away disappointed. But if you’re ready to understand your pain, you might find your freedom.
Real stories: What patients say
On Reddit’s chronic pain community, one user wrote: “I spent six months terrified to move. I thought my spine would collapse if I bent over. Then I learned my pain was like a smoke alarm set off by toast. I started walking again. Now I hike. I cut my pain meds by 75%.”
A 42-year-old nurse with fibromyalgia went from six pain pills a day to one every three days after six PNE sessions and a gradual return to activity. She didn’t become pain-free. But she became functional again.
Not everyone has success. About 17% of patient reviews mention feeling overwhelmed by the science. Others say it didn’t help their acute pain. That’s okay. PNE isn’t for everyone. But for those who connect with it, it changes everything.
How to get started
PNE is now part of standard care in 68% of U.S. physical therapy clinics focused on pain. In the UK, it’s growing fast, especially in NHS pain clinics and private physio practices.
You don’t need a referral. Just ask your physiotherapist: “Do you offer Pain Neuroscience Education?” If they say no, ask if they’ve heard of the “Explain Pain” approach by David Butler and Lorimer Moseley. That’s the most common version.
If your provider isn’t trained, look for clinics that specialize in chronic pain. Many offer group PNE courses. Some even have digital tools like the “Pain Revolution” app, used by over 180,000 people.
And if you’re a clinician? Start small. Learn the basics. Use simple metaphors. Practice explaining pain like you’re talking to a friend. You don’t need a fancy certification. You just need to believe that pain isn’t always about damage-and that knowledge can heal.
What’s next for pain education
Researchers are now testing PNE for post-surgical pain. Early results show it can reduce opioid use and speed up recovery. Virtual reality is being used to teach pain biology in immersive ways-patients “walk through” their nervous system in 3D. One trial found VR learners retained 30% more than those who just listened.
Insurance is catching up too. In the U.S., Medicare now covers PNE under physical therapy codes. Employers are using it: 41 Fortune 100 companies have added PNE to their injury programs, cutting workers’ comp claims by 22%.
But the biggest change isn’t in tech or policy. It’s in mindset. More people are realizing: pain doesn’t have to be a life sentence. Understanding it is the first step to taking it back.


Solomon Ahonsi
February 1, 2026 AT 12:51George Firican
February 2, 2026 AT 13:05Matt W
February 3, 2026 AT 08:31Anthony Massirman
February 3, 2026 AT 17:18Brittany Marioni
February 4, 2026 AT 18:05Dan Pearson
February 5, 2026 AT 23:52Marc Durocher
February 6, 2026 AT 15:57larry keenan
February 7, 2026 AT 09:15Nick Flake
February 7, 2026 AT 17:56Akhona Myeki
February 9, 2026 AT 12:45Brett MacDonald
February 10, 2026 AT 00:35Sandeep Kumar
February 10, 2026 AT 08:14