When you pick up a prescription, you might see two names on the label: one you recognize, like Lyrica, and another you’ve never heard of, like pregabalin. The second one is the generic version - same drug, same effect, but often a fraction of the price. In 2022, Americans saved $408 billion just by choosing generics over brand-name drugs. That’s not a guess. That’s a fact from IQVIA’s official savings report. And it’s not just about saving a few dollars here and there - it’s about making healthcare affordable for millions.
Why Generics Cost So Much Less
Generic drugs aren’t cheap because they’re low quality. They’re cheap because they don’t need to repeat the billion-dollar research and clinical trials that brand-name drugs do. When a company invents a new medicine, they get a patent that protects them from competition for 20 years. Once that patent expires, other manufacturers can produce the same drug using the same formula. They don’t need to prove it works again - the FDA already did. All they have to show is that their version delivers the same amount of active ingredient into the bloodstream at the same rate. That’s called bioequivalence, and it’s measured between 80% and 125% of the brand’s performance. If it’s in that range, it’s approved.The result? A single generic version of a drug can cut the price by 80% or more. When multiple companies start making it, prices drop even further. For example, the brand-name antidepressant Prozac (fluoxetine) used to cost over $200 a month. Today, the generic version costs under $10. That’s not a sale. That’s how the system is supposed to work.
Real Numbers, Real Savings
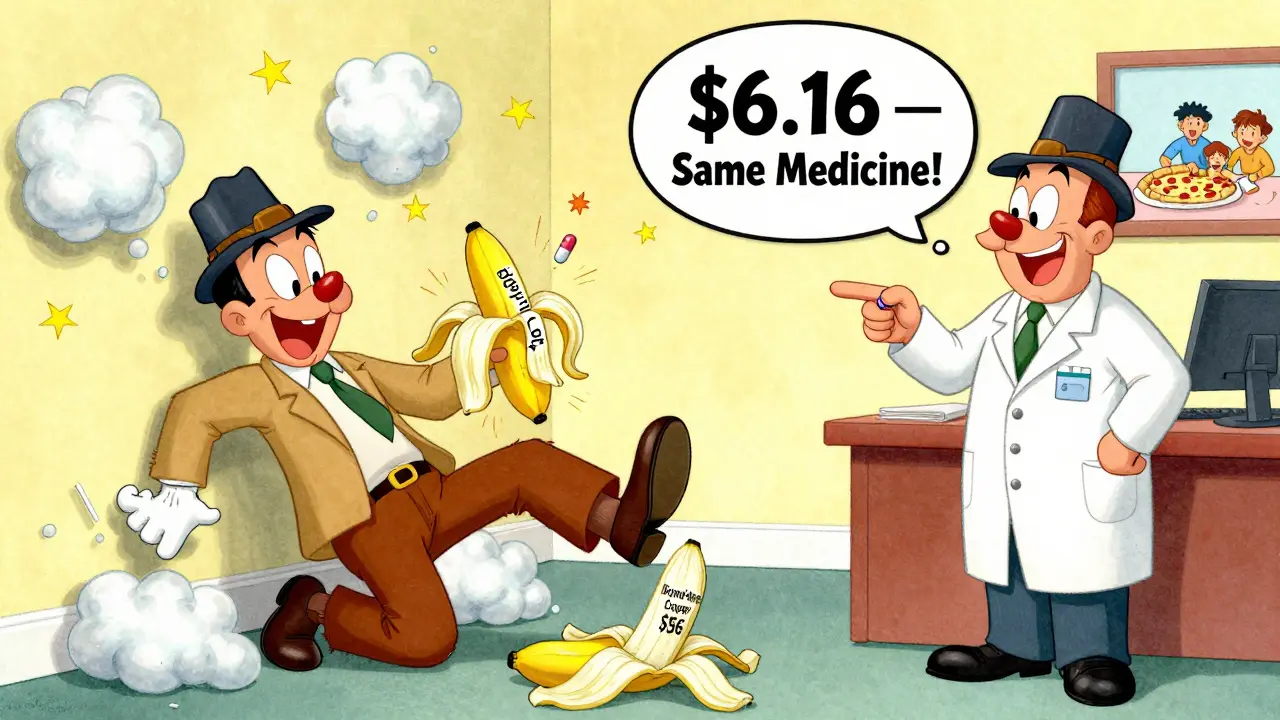
Let’s break down what this looks like at the pharmacy counter. In 2023, the average copay for a generic prescription was $6.16. For the brand-name version of the same drug? $56.12. That’s more than nine times more. And it’s not just a one-time difference. Over a year, someone taking a monthly generic instead of the brand could save over $600. Multiply that by millions of people, and you get the $408 billion in savings reported for 2022.Even more striking: generics make up 90% of all prescriptions filled in the U.S., but they account for only 1.5% of total drug spending. Brand-name drugs, which are prescribed far less often, still take up nearly 85% of the money spent on prescriptions. That’s the power of scale and competition. The more generic manufacturers enter the market, the lower the price goes.
Therapeutic Substitution: The Hidden Savings
Most people think savings come from swapping a brand for its direct generic. But the biggest savings often come from switching to a different generic altogether. A 2022 study from Johns Hopkins looked at the top 1,000 generic drugs in Colorado and found that some generics were being sold for 15 times the price of another generic that worked just as well. For example, one version of the blood pressure drug amlodipine cost $120 a month, while another version - same active ingredient, same dose - cost just $8. That’s a 93% discount just by choosing a different generic.This isn’t rare. The study found 45 high-cost generics that had cheaper therapeutic alternatives. On average, switching saved patients 88.3% per prescription. These savings don’t require a new doctor’s note. Often, pharmacists can recommend the lower-cost option if you ask. You just need to know to ask.

What About Safety and Effectiveness?
A lot of people worry that generics aren’t as good. They’ve heard stories about someone who switched to a generic and felt different. But here’s the truth: the FDA requires generics to meet the same strict standards as brand-name drugs. The same factories often make both versions - just under different labels. In fact, more than 98% of FDA-approved generics are rated “AB,” meaning they’re therapeutically equivalent.There are exceptions. For drugs with a narrow therapeutic index - like levothyroxine (for thyroid), warfarin (for blood thinning), or some epilepsy meds - even tiny differences in absorption can matter. That’s why some doctors prefer to stick with one brand or generic for these drugs. But even here, the problem isn’t the generic itself. It’s inconsistent switching between different generic manufacturers. If you’re stable on one version, don’t switch unless your doctor says to.
Harvard Medical School surveyed doctors in 2023 and found that when they explained the FDA’s bioequivalence rules to patients, 87% of concerns disappeared. Most fears come from misunderstanding, not experience.
Who’s Saving the Most?
Medicare beneficiaries fill 91% of their prescriptions with generics - the highest rate of any group. Yet, 41% still struggle to afford them. Why? Because even $10 a month adds up. A $30 copay for a generic isn’t cheap if you’re on a fixed income. That’s why the 2023 Inflation Reduction Act capped Medicare Part D out-of-pocket costs at $2,000 a year. It’s not just about generics being cheap - it’s about making sure people can actually use them.On the private insurance side, the savings are even clearer. Between 2010 and 2020, out-of-pocket payments for generics dropped by about 50%. The total cost - what you pay plus what your insurer pays - fell by nearly 80%. That’s not just good for patients. It’s good for employers, insurers, and the whole system.
Why Aren’t We Using More Generics?
If generics are this effective, why do brand-name drugs still exist? Because the system isn’t perfect. Some drugmakers use legal tricks - like filing dozens of minor patents - to delay generic entry. The FTC found that brand companies file an average of 17.5 patents per drug just to block competition. Others pay generic makers to stay off the market - a practice called “pay-for-delay” - which the FTC is now cracking down on.Another problem? Drug shortages. In September 2023, there were 312 active shortages in the U.S., and 78% of them were for generic drugs. That’s because generic manufacturers often operate on thin margins. If one factory has a problem, there’s no backup. That’s why some pharmacies run out of the cheapest version and have to give you the more expensive one - not because it’s better, but because it’s the only one in stock.
What You Can Do Right Now
You don’t need a degree in pharmacy to save money. Here’s what works:- Always ask: “Is there a generic version?” Even if your doctor doesn’t mention it, you can request it.
- Ask your pharmacist: “Is there a cheaper generic alternative?” Sometimes the one you’re getting isn’t the cheapest.
- Use tools like GoodRx or SingleCare. They show real-time prices at nearby pharmacies - and often the lowest price is for a generic.
- Don’t assume your insurance covers the cheapest version. Sometimes you can pay cash for a generic and save more than your copay.
- If you’re on a chronic medication, ask your doctor about therapeutic substitution. You might be able to switch to a different generic that’s just as effective but costs 90% less.
One Reddit user shared they paid $450 for the brand-name version of sertraline. The generic? $9. That’s not a lucky break - that’s how the system works when you use it right.
The Bigger Picture
The U.S. pays 2.78 times more for prescription drugs than other wealthy countries. Generics are the reason we don’t pay even more. Without them, drug spending would be unaffordable for most people. They’re not a Band-Aid. They’re the backbone of affordable care.By 2025, generics are expected to save the U.S. healthcare system over $425 billion annually. That’s money staying in people’s pockets, not going to pharmaceutical marketing or executive bonuses. It’s not magic. It’s competition. It’s transparency. It’s the simple idea that if two drugs do the same thing, they should cost the same.
Next time you get a prescription, don’t just take the first name on the label. Ask. Compare. Save. Your wallet - and your health - will thank you.
Are generic medications as effective as brand-name drugs?
Yes. The FDA requires generic drugs to have the same active ingredient, strength, dosage form, and route of administration as the brand-name version. They must also prove bioequivalence - meaning they deliver the same amount of medicine into your bloodstream at the same rate. Over 98% of generics are rated "AB" by the FDA, meaning they’re therapeutically equivalent. Millions of people use generics safely every day.
Why do some people say generics don’t work for them?
In rare cases, people report differences when switching between generics or from brand to generic - especially with drugs like levothyroxine or warfarin, where small changes in blood levels matter. But this is usually because they switched between different generic manufacturers, not because generics are inferior. The solution? Stick with one manufacturer once you find one that works. If you notice changes, talk to your doctor or pharmacist before switching again.
Can pharmacists switch my brand-name prescription to a generic without asking?
In 49 U.S. states, pharmacists can automatically substitute a generic for a brand-name drug unless the doctor writes "dispense as written" or "no substitution." New York is the only state that requires the prescriber to specifically allow substitution. Even then, pharmacists are trained to suggest the most cost-effective option - and they’re required to tell you if a cheaper generic is available.
Why are some generic drugs more expensive than others?
Not all generics are priced the same. When a new generic enters the market, prices drop fast. But if only one company makes it, or if there’s a shortage, the price can stay high. That’s why you might pay $15 for one version of a drug and $3 for another. Always ask your pharmacist: "Is there a lower-cost generic available?" You’d be surprised how often the answer is yes.
Do insurance plans encourage the use of generics?
Yes. Most insurance plans have tiered copays - generics are usually in Tier 1, meaning the lowest cost. Brand-name drugs are often Tier 2 or 3, with higher copays or even prior authorization requirements. Some plans won’t cover a brand-name drug at all unless you’ve tried the generic first. This isn’t just to save money - it’s because generics are proven to be just as safe and effective.
What’s the difference between a generic and a biosimilar?
Generics are exact copies of small-molecule drugs - pills or injections made of simple chemicals. Biosimilars are copies of complex biologic drugs - made from living cells, like insulin or rheumatoid arthritis treatments. Biosimilars aren’t identical, but they’re highly similar and work the same way. They’re newer, more expensive to make, and not as widely used yet. But they’re starting to save billions too - $3.2 billion in 2023 alone.
How can I find the cheapest generic version of my medication?
Use free tools like GoodRx, SingleCare, or Blink Health. Enter your drug name and zip code - they’ll show you prices at nearby pharmacies. Often, the cash price for a generic is lower than your insurance copay. You can also ask your pharmacist to check the FDA’s Orange Book or AAM’s formulary tools to find the lowest-cost option. Don’t assume your first prescription is the cheapest one.





Siobhan Goggin
January 4, 2026 AT 12:30Just filled my prescription yesterday and paid $7 for a month’s supply of generic sertraline. Last year it was $45. I didn’t even ask for the generic - the pharmacist just handed it over and said, ‘You’re saving a fortune.’ That’s the system working right.
Roshan Aryal
January 6, 2026 AT 00:32Let’s be real - this whole generic thing is just corporate greed dressed up as ‘savings.’ The FDA approves generics based on bioequivalence? That’s a joke. What’s ‘equivalent’ when your body reacts differently? And don’t get me started on how Indian and Chinese factories are flooding the market with cheap pills that have fillers no one talks about. You think you’re saving money? You’re just gambling with your health.
Vicki Yuan
January 6, 2026 AT 01:05Actually, the FDA’s bioequivalence standard of 80–125% is scientifically rigorous - it’s based on pharmacokinetic studies with hundreds of participants. If a generic falls outside that range, it’s rejected. The system isn’t perfect, but it’s not a scam. The real issue is inconsistent switching between manufacturers, especially for narrow-therapeutic-index drugs. Stick with one version once you find what works.
Ethan Purser
January 6, 2026 AT 03:35Oh wow, so we’re supposed to be grateful that corporations let us buy our own medicine at 10% of the price? This isn’t generosity - it’s capitalism finally letting a little air in after 20 years of price gouging. And yet, people still act like generics are some kind of charity. They’re not. They’re the natural consequence of patents expiring. The real villain is the pharma lobby that fights to extend those patents with 17.5 lawsuits per drug. Don’t thank the system - fight it harder.
Dee Humprey
January 7, 2026 AT 13:49My mom’s on warfarin. She switched generics once and her INR went wild. Now she only takes the one brand her pharmacist recommends - even though it’s $15 instead of $5. She says, ‘Better safe than sorry.’ And honestly? She’s right. For some meds, consistency matters more than cost. Don’t switch unless you have to.
Jacob Milano
January 8, 2026 AT 04:49I used to think generics were sketchy until I started tracking my blood pressure meds. I switched from brand to generic - same doctor, same dose, same pharmacy. My numbers didn’t budge. I saved $500 a year. Now I ask every time: ‘Is there a cheaper one?’ Most pharmacists are happy to help. It’s not complicated. Just ask.
Uzoamaka Nwankpa
January 8, 2026 AT 22:00I wish this was true where I live. Here, the generic is always out of stock. The pharmacy gives me the brand-name and says, ‘Insurance won’t cover the generic right now.’ But I know they’re just running low because no one wants to make it anymore. Thin margins. No incentive. We’re all stuck paying more because no one wants to risk losing money on pills.
John Wilmerding
January 9, 2026 AT 12:36It is worth noting that the 90% prescription volume for generics, coupled with their 1.5% share of total drug expenditure, underscores a remarkable efficiency in pharmaceutical distribution. This is not merely a cost-saving measure - it is a structural optimization of healthcare delivery. The market dynamics at play here are both economically sound and ethically defensible.
Stephen Craig
January 9, 2026 AT 15:40Generics work. But the system doesn’t reward transparency. Why do some cost 15x more? Because no one checks. People just take what’s handed to them. That’s the real problem.
Charlotte N
January 10, 2026 AT 18:44So i just found out my generic lisinopril costs $3 at walmart but $22 at my usual pharmacy... and my insurance didn't even tell me... why is this so hard to figure out??
Catherine HARDY
January 11, 2026 AT 19:28Did you know the FDA lets companies use the same labs to test their own generics? That’s not oversight - that’s a conflict of interest. And what about the fillers? Talc, dyes, corn starch - all kinds of junk that can trigger allergies. They don’t test for that. They just test ‘bioequivalence.’ That’s not medicine - that’s a loophole.
bob bob
January 12, 2026 AT 11:28I used to be scared of generics too - until I switched to the $4 version of metformin and didn’t die. Turns out, my body didn’t care. Now I tell everyone: ‘Ask for the cheapest one. Worst case, you save money. Best case, you live longer.’
Akshaya Gandra _ Student - EastCaryMS
January 12, 2026 AT 15:18im a student in india and we use generics all the time here they r way cheaper and work fine but i heard in usa its different? like the quality??
mark etang
January 13, 2026 AT 16:42As a healthcare economist, I must emphasize that the $408 billion in annual savings attributable to generic drug utilization represents not merely a fiscal benefit, but a profound societal equity intervention. Access to affordable therapeutics is a determinant of health outcomes as critical as clinical efficacy. The continued expansion of generic market penetration - particularly among Medicare and low-income populations - must be actively supported through policy, education, and pharmacist empowerment.
Jack Wernet
January 15, 2026 AT 02:31My father was prescribed levothyroxine for 15 years. He switched generics three times - each time, his TSH levels fluctuated. Eventually, he went back to the brand. His doctor said, ‘It’s not about the drug. It’s about consistency.’ He’s fine now. I wish more people knew that.